ABSTRACT
- Cardiovascular disease (CVD) is the most frequently diagnosed disease as well as the leading cause of death in the elderly. It usually results from long-term effects of cardiovascular risk factors as well as the aging process itself. Elderly people commonly have geriatric syndrome, which is an age-specific problem that is complicated by the presence of cardiovascular, cognitive, and physical dysfunction and is accompanied by many other chronic diseases. While caring for the elderly, in addition to CVD, various inherent problems must be considered. The patient-centered approach, instead of evidence-based guidelines that are designed for young adult patients, is the most important concept when it comes to elderly patients with CVD and multiple comorbidities. This approach should be used to maintain the functionality, independence, quality of life, and dignity of these patients.
-
Keywords: Aging; Cardiovascular diseases; Frail elderly; Frailty; Geriatric assessment
Cardiovascular disease (CVD) is the most frequently diagnosed disease and the leading cause of death in the elderly. Excluding a few, most CVDs in the elderly are caused by a combination of physiological changes due to aging and pathological changes related to longterm exposure to cardiovascular risk factors.1)2) Elderly people often have geriatric syndrome, which is a age-related problem that includes the overall aging of the organs in addition to cardiovascular, cognitive, and physical dysfunction. Geriatric syndrome is often accompanied concurrently by several chronic diseases. Therefore, when treating elderly patients with CVD, it is necessary to formulate an individualized, patient-centric treatment strategy, taking into account various factors, including an evaluation of the overall systemic condition, life expectancy, co-morbid diseases, and the patient's wishes for treatment goals.
AGING-RELATED CHANGES IN THE CARDIOVASCULAR SYSTEM
- Normal and healthy endothelial cells in the blood vessels secrete nitric oxide (NO), prostacyclin, and bradykinin to maintain a vasodilatory state and inhibit thrombus formation. When vascular endothelial cells are damaged due to prolonged exposure to cardiovascular risk factors, the concentration of inflammatory mediators and the expression of angiotensin II in tissues increases, which results in an increased tendency for vasoconstriction, endothelial cell permeability, platelet aggregation, leukocyte adhesion, and cytokine production. Furthermore, cholesterol is known to penetrate the blood-vessel lining. Cardiovascular risk factors, such as diabetes and smoking, can lead to the formation of atherosclerotic plaques on the arterial wall also found in CVDs, even at a younger age. Although one cannot have a specific cardiovascular risk factor, extended exposure to high concentrations of lipidemia, low-density lipoprotein cholesterol (LDL-C) >8 g/dL per year or more, is enough to cause CVD by atherosclerosis due to the accumulation of risk factors in the elderly (Figure 1).3)
- Ageing-related changes in the arterial media include thickening, decreased elastic fibers, and increased collagen deposition, which are age-related medial degeneration and sclerosis, resulting in increased arterial stiffness. In most cases of endothelial cell dysfunction, blood vessels tend to contract, which increases both systolic and diastolic blood pressure. Moreover, arterial stiffness is a major pathological cause of increased systolic blood pressure (BP). The systolic BP reading raised from a value of 50 to 60 when there was an increase in arterial stiffness. Whereas diastolic BP decreased as arterial stiffness became more severe.4-6)
- A commonly seen aging-related change is the ventricular hypertrophy, which mainly affects the left ventricle. With aging, cardiomyocytes decrease in number due to either necrosis or apoptosis; however, each cardiomyocyte becomes thickened, collagen fibers are deposited, and other non-cardiomyocyte cells such as adipocytes infiltrate around these cells, all of which result in ventricular hypertrophy. The absolute number of ventricular cardiomyocytes gradually decreases with age, resulting in reduced contraction of the ventricles and possible heart failure. Left ventricular ejection fraction (EF) at rest is mostly in normal range, it is usually diagnosed as “heart failure with preserved ejection fraction (HFpEF)”. In HFpEF, accompanying aging of the cardiac conduction system impairs the ability to physiologically increase heart rate on demand, and thus ventricular relaxation dysfunction impairs sufficient cardiac output. Therefore, heart failure can occur during exercise as well as normal daily activities. HFpEF is observed in 40–80% of the elderly and is more commonly found in women.7)8)
- The age-related changes that affect the aortic valve leaflets are usually fibrosis and calcification. The aortic valve repetitively opens and closes approximately 100,000 times per day while pumping blood. Minute mechanical damage accumulates over time, resulting in degenerative changes. At an early stage, the change is termed sclerosis. Moreover, aortic valve stenosis (AS) is the most problematic valvular heart disease in the elderly.9)
AGING CHANGES IN DRUG METABOLISM
- Pharmacokinetics refers to the absorption, distribution, metabolism, and excretion of drugs in the body. Whereas, pharmacodynamics is the study of physiological and biochemical effects of drugs on the body. Changes in pharmacokinetics and pharmacodynamics may occur due to physiological changes associated with aging. As more drugs are taken, these changes can get more complex and result in increased drug-related side effects.10)11) Since most cardiovascular drugs are absorbed through passive diffusion, the total amount absorbed by the digestive tract remains almost unchanged despite gastrointestinal aging. However, drug distribution in the body is significantly affected by aging. Changes in body composition that may alter the volume of distribution in elderly patients include a decrease in total body water and an increase in fat content. Since water-soluble drugs such as digoxin have a decreased volume of distribution in the elderly, the blood concentration may be higher even if the same amount of the drug is administered. Conversely, fat-soluble drugs, such as amiodarone, have an increased volume distribution, thus increasing half-life.
- The most important change in aging-related pharmacokinetics is the decrease in drug metabolism and excretion. In general, the glomerular filtration rate decreases by 10% every 10 years in both men and women. Elderly patients with decreased muscle mass may have serum creatinine levels within the normal range, 0.8–1.3 mg/dL, but have significantly compromised renal function. Therefore, the glomerular filtration rate is calculated using the Cockroft-Gault calculation formula that considers age, sex, weight, and the dosage of drugs excreted to the kidneys. Drug metabolism in the liver is influenced by several processes that involve hepatic blood flow and enzyme activity of hepatocytes. During aging, drug metabolism in hepatocytes is maintained at a stable rate. However, primary metabolism by cytochrome P-450 is affected when hepatic blood flow decreases. Concomitant diseases, a situation in which blood flow to the liver is reduced and drugs that affect liver metabolism are administered concurrently, the primary metabolism may be affected and the half-life may be altered. However, this has been difficult to confirm clinically.
- With age, the sensitivity of baroreceptors and β-receptors has been known to decrease. Reduction of baroreceptor sensitivity in the elderly increases the likelihood of orthostatic hypotension due to blockage of the compensatory response when non-dihydropyridine calcium blockers are administered. This a pharmacodynamic related change.12)13) For these reasons, it is important to start with a small dose and increase slowly to avoid prescribing several drugs at the same time, familiarize the elderly with interactions between drugs and foods, and check whether the occurrence of side effects.
AGING-RELATED CHANGES IN SYSTEMIC CONDITIONS
- The atypical deterioration of health that occurs due to the accumulation of various organ disorders due to aging in the elderly is called geriatric syndrome. An elderly patient whose chief complaint is a result of a geriatric syndrome will often present with symptoms that are difficult to attribute to the organ system that caused the initial pathology. Symptoms of geriatric syndrome include delirium, issues with balance, urinary incontinence, dizziness, sleep disturbance, and frailty (Figure 2). Since these symptoms are non-specific, a comprehensive geriatric assessment (CGA) is required for appropriate treatment. CGA includes evaluation of audiovisual function, nutritional status, urinary function, gait disorder, fall risk, multi-drug use, cognitive/emotional function, basic/instrumental activities of daily living, physical function, and social support. In other words, the test is used to evaluate elderly patients who visit with atypical symptoms, including geriatric syndrome, where the expression of symptoms is ambiguous and cognitive dysfunction is impaired. Therefore, it is necessary to take sufficient time to understand the complaints used by the patient in a comfortable state.
FRAILTY
- Old age refers to a condition in which the physiological reserve of various organs is reduced, and is thus vulnerable to general stress. The decrease in bodily function mainly occurs due to negative interactions between important organs of the body, such as the musculoskeletal system, the immune system, and the neuroendocrine system; for example, sarcopenia is considered an important cause for such decrease. Frailty is a major symptom of geriatric syndrome and a major prognostic factor for CVD in the elderly. Elderly people in a senile state are vulnerable to general stress, and their dependence on others increases while going through their daily lives. When frailty worsens, irreversible disability occurs, as a result, hospitalization increases, they cannot return home and die while staying in nursing homes.
- In the aging population, CVD as well as frailty are common and often coexist. It is possible that cardiovascular risk factors simultaneously act as well for frailty.14) It is, therefore, important to establish an appropriate treatment strategy for individual patients as those who are frail, alongside having CVD, would not be able to tolerate the generic drug or surgical treatment process well, and hence the resultant damage may be greater than the benefit. Furthermore, there are no standardized measurement tools for assessing frailty. The Clinical Frailty Scale is subjective and inaccurate in evaluating the function and general condition of the elderly through the subjective eye-ball assessment (Figure 3).15) The criteria developed by Fried et al.,16) 2001, is the most widely cited form of assessment (Table 1), where if three or more of the 5 criteria (weight loss, extreme fatigue, muscle weakness, walking speed, and physical activity that can be standardized) are satisfied, it is defined as frailty. However, since the Fried frailty index's definition is not suitable for the elderly with CVD, more systematic and simple measurement tools for each disease is being studied.17)
CHARACTERISTICS OF CVD IN THE ELDERLY
- The prevalence of coronary artery disease, atrial fibrillation, and heart failure greatly increases with age. Meanwhile, issues such as isolated systolic hypertension, severe aortic valve stenosis, and senile cardiac amyloidosis are also known to occur in the elderly. CVD is often a precursor of functional decline, weakness, decreased independence, and disability. In elderly patients, the disease is often accompanied by a decrease in body-mental performance. These changes, although individual differences, appear in almost all older adults after the age of 80 and worsens rapidly. In those who suffer from frailty due to aging, the susceptibility to various diseases, including CVD, increases; therefore, they often suffer from various other chronic diseases. This multi-morbidity condition causes an overall decline in function through the interaction of the various diseases, lowering the quality of life, and increasing the risk of other complications. Moreover, there is a high risk of adverse reactions to treatment, including drugs, as well as an increase in mortality during hospitalization and treatment (Figure 4).
- In patients with cases of multi-morbidity, evidence-based therapeutic drugs are prescribed for each disease; hence, the use of polypharmacy is common. In elderly people with somatic homeostasis that is caused due to aging, age itself is a big risk factor for adverse drug reactions, and since multiple drugs are administered due to multiple morbidities, the risk of side effects rapidly increase due to various drug-drug and drug-disease interactions. Nonsteroidal anti-inflammatory drugs commonly prescribed for degenerative arthritis reduces the effects of antihypertensive drugs, increasing side effects. They can also cause heart and kidney dysfunction, but since the degree is mild, it is not a major problem for healthy people. However, in the elderly, side effects can synergistically create a vicious cycle, which can significantly worsen health.18)
GENERAL PRINCIPLES FOR THE TREATMENT OF CVDs IN THE ELDERLY
- In the presence of cardiovascular risk factors in young adults, the risk of developing diseases increases, and it is important to prevent CVD through lifestyle modification. However, in the elderly, lifestyle habits are prominent, while CVDs are already present as well as targeted organ damage. Thus, there is a hurdle to expect sufficient therapeutic effects only through lifestyle modifications. The risk of CVD increases proportionally with higher blood pressure, blood glucose, and cholesterol concentrations in young adults. In the elderly, however, the mortality rate increases even in patients with very low blood pressure, blood glucose, and cholesterol levels. Such a “J-curve phenomenon” exists because, in the elderly patients with advanced CVDs, significant malnutrition related to chronic wasting diseases decrease blood pressure, blood glucose, and cholesterol. Therefore, those with CVDs and systemic issues, treatment for co-morbid diseases, nutritional support, and non-drug treatment such as rehabilitation treatment for functional recovery must be combined.19)20)
- The elderly are at a high risk of hemorrhagic side effects when administered antithrombotic drugs. The HAS-BLED bleeding risk score is a tool used to assess the risk of bleeding in patients with atrial fibrillation during warfarin administration. One point is given each for the presence of hypertension, abnormal kidney and liver function, previous stroke or bleeding history, fluctuation in international normalization ratio (INR) levels, advanced age, chronic medication, and alcohol consumption. A total of 3 points or more is considered a high-risk group for bleeding.21) Elderly patients with CVD often have abnormal renal or hepatic function, multi-morbidity, prolonged use of drugs such as nonsteroidal antiinflammatory drugs that increase bleeding tendency, and multi-drug use resulting in increased INR variability. Therefore, warfarin should be administered with maximal caution and surveillance.
- Polypharmacy in the elderly is often caused by not only multiple comorbidities but also the “prescribing cascade” pattern, which refers to a prescription of a second drug to treat the symptoms of a drug side effect by mistaking it as a symptom of another disease. Inappropriate polypharmacy imposes a substantial burden of adverse drug events, ill-health, disability, hospitalization, and even death. The most important predictor of adverse drug events in older patients is the number of prescribed drugs. To reduce side effects caused by unnecessary or excessive drugs, the goal of treatment should be prioritized, and the number of prescribed drugs should be minimized. In the elderly, the process of “de-prescription” to reduce unnecessary drugs is essential. Even those that have been proven to be effective should be monitored for side effects and regularly checked for the need for reduction or discontinuation.22)
- Most of the “evidence-based” disease treatment guidelines are based on studies that have selected a single disease population without comorbidities to focus on one disease or a single organ and exclude interactions between multiple diseases. Many of these studies do not include elderly patients.23) Therefore, uniform treatment under “evidence-based” guidelines may not only solve but even worsen the number of comorbidities in elderly patients who have taken multiple drugs for multiple diseases. For elderly patients with a poor general condition, short life expectancy, multiple comorbidities, or significant geriatric syndrome such as frailty, treatment needs to be individualized rather than applying a single disease-based treatment guideline. Avoiding side effects should be prioritized.
- Elderly patients with CVD may already have targeted organ damage and complications, advanced co-morbid diseases, or even decreased physiologic reserves, all of which may not withstand the standard treatment processes according to evidence-based guidelines. For example, open-heart surgery is the standard treatment for severe ischemic heart disease or severe aortic valve stenosis with reduced left ventricular systolic function. However, many elderly patients with poor general health cannot tolerate the stress of such surgical procedures and have a high treatment-related mortality rate. Even if the treatment itself is successful, the whole-body condition often deteriorates during the treatment process to an irreversible independent daily life. It is common for such patients to stay in nursing facilities for the rest of their lives. Therefore, it is more important to preserve life functions as much as possible so that they can continue to live independently rather than cure certain diseases. Hence, when choosing a treatment strategy for the elderly, the risk should be assessed differently from that of young adults, considering the presence of co-morbid diseases, physical function, basic activities of daily living, instrumental activities of daily living, and frailty. Through the patient-centered approach, wishes for their remaining time should be prioritized to improve quality of life.
SUMMARY
- A patient-centered approach is the most important concept when it comes to caring for elderly patients with CVD and multiple comorbidities in which medical, functional, and psychosocial problems are complicated. It is important to focus on maintaining the functionality, independence, quality of life, and dignity of elderly patients in the decision-making process before applying routine recommendations from evidence-based guidelines.
ARTICLE INFORMATION
-
Conflict of Interest
The author has no financial conflicts of interest.
Fig. 1.
Threshold for atherosclerotic cardiovascular disease as a function of cumulative LDL-C exposure. Modified from Ference et al.3)
CV = cardiovascular; CVD = cardiovascular diseases; FH = familial hypercholesterolemia; LDL-C = low-density lipoprotein cholesterol.

Fig. 2.Occurrence of frailty, geriatric syndrome, and disease due to aging.
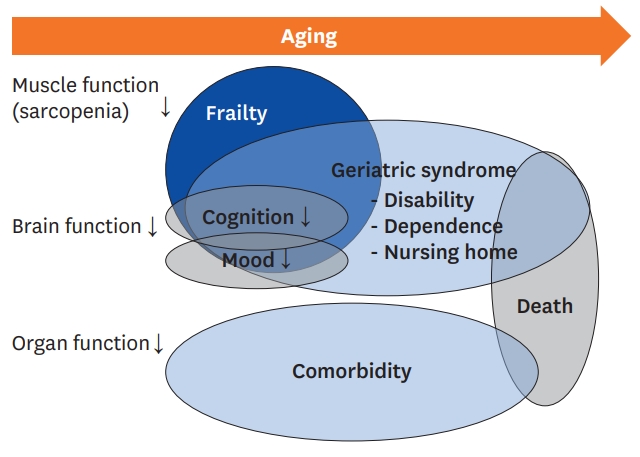
Fig. 3.
Clinical frailty scale.
Figure has modified from the Canadian Study on Health & Aging, Revised 2008.

Fig. 4.Features of elderly patients with cardiovascular diseases.
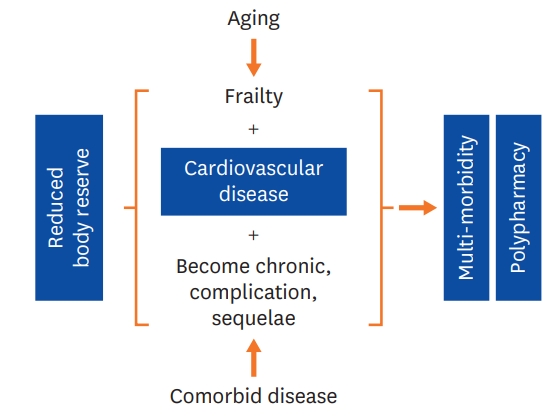
Table 1.Fried frailty index
|
Frailty criteria |
Indicators |
|
Shrinking (weight loss) |
Baseline >4.5 kg of unintentional weight loss over the past year |
|
Exhaustion |
Self-reported exhaustion for over ≥3 days of the week |
|
Weakness |
Maximal grip strength using a handheld dynamometer (kg); lowest 20% stratified by gender and BMI quartiles |
|
Slowness |
Time to walk=4.5 m at usual pace (sec); slowest 20% stratified by gender and height |
|
Low physical activity |
Inability to perform ≥moderate activity in the past 2 weeks |
REFERENCES
- 1. Forman DE, Rich MW, Alexander KP, Zieman S, Maurer MS, Najjar SS, Cleveland JC Jr, Krumholz HM, Wenger NK. Cardiac care for older adults. Time for a new paradigm. J Am Coll Cardiol 2011;57:1801–10.PubMedPMC
- 2. Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation 2003;107:346–54.ArticlePubMed
- 3. Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: JACC health promotion series. J Am Coll Cardiol 2018;72:1141–56.PubMed
- 4. Fleg JL, Strait J. Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart Fail Rev 2012;17:545–54.ArticlePubMedPMC
- 5. Fritze O, Romero B, Schleicher M, Jacob MP, Oh DY, Starcher B, Schenke-Layland K, Bujan J, Stock UA. Age-related changes in the elastic tissue of the human aorta. J Vasc Res 2012;49:77–86.ArticlePubMed
- 6. Meyer ML, Tanaka H, Palta P, Cheng S, Gouskova N, Aguilar D, Heiss G. Correlates of segmental pulse wave velocity in older adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens 2016;29:114–22.ArticlePubMed
- 7. Lloyd-Jones DM, Larson MG, Leip EP, Beiser A; D'Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ; Levy D; Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation 2002;106:3068–72.ArticlePubMed
- 8. Redfield MM. Heart failure with preserved ejection fraction. N Engl J Med 2016;375:1868–77.ArticlePubMed
- 9. Iung B, Vahanian A. Degenerative calcific aortic stenosis: a natural history. Heart 2012;98 Suppl 4:iv7–13.ArticlePubMed
- 10. Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev 2009;41:67–76.ArticlePubMed
- 11. Sera LC, McPherson ML. Pharmacokinetics and pharmacodynamic changes associated with aging and implications for drug therapy. Clin Geriatr Med 2012;28:273–86.ArticlePubMed
- 12. Montamat SC, Abernethy DR. Calcium antagonists in geriatric patients: diltiazem in elderly persons with hypertension. Clin Pharmacol Ther 1989;45:682–91.ArticlePubMed
- 13. White M, Roden R, Minobe W, Khan MF, Larrabee P, Wollmering M, Port JD, Anderson F, Campbell D, Feldman AM. Age-related changes in beta-adrenergic neuroeffector systems in the human heart. Circulation 1994;90:1225–38.ArticlePubMed
- 14. Stewart R. Cardiovascular disease and frailty: what are the mechanistic links? Clin Chem 2019;65:80–6.ArticlePubMed
- 15. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–95.ArticlePubMedPMC
- 16. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G; McBurnie MA; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56.ArticlePubMed
- 17. Afilalo J, Lauck S, Kim DH, Lefèvre T, Piazza N, Lachapelle K, Martucci G, Lamy A, Labinaz M, Peterson MD, Arora RC, Noiseux N, Rassi A, Palacios IF; Généreux P, Lindman BR, Asgar AW, Kim CA, Trnkus A, Morais JA, Langlois Y, Rudski LG, Morin JF, Popma JJ, Webb JG, Perrault LP. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR study. J Am Coll Cardiol 2017;70:689–700.PubMed
- 18. Boparai MK, Korc-Grodzicki B. Prescribing for older adults. Mt Sinai J Med 2011;78:613–26.ArticlePubMed
- 19. Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med 2012;172:1162–8.PubMedPMC
- 20. Félix-Redondo FJ, Grau M; Fernández-Bergés D. Cholesterol and cardiovascular disease in the elderly. Facts and gaps. Aging Dis 2013;4:154–69.PubMedPMC
- 21. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010;138:1093–100.ArticlePubMed
- 22. Scott IA, Hilmer SN, Reeve E, Potter K, Le Couteur D, Rigby D, Gnjidic D, Del Mar CB, Roughead EE, Page A, Jansen J, Martin JH. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med 2015;175:827–34.ArticlePubMed
- 23. Feldman RD, Harris SB, Hegele RA, Pickering JG, Rockwood K. Applying atherosclerotic risk prevention guidelines to elderly patients: a bridge too far? Can J Cardiol 2016;32:598–602.ArticlePubMed
Citations
Citations to this article as recorded by

- Assessment of Quality of Life in Patients With Cardiovascular Disease Using the SF-36, MacNew, and EQ-5D-5L Questionnaires
Aikaterini Chatzinikolaou, Stergios Tzikas, Maria Lavdaniti
Cureus.2021;[Epub] CrossRef



