Aspirin Has a Neutral Effect in Preventing Future Cardiovascular Events in Vasospastic Angina
Article information
Abstract
Background
The aim of this multi-center prospective registry study was to evaluate the clinical efficacy of low-dose aspirin in vasospastic angina (VA) patients for the prevention of future cardiovascular events.
Methods
A total of 1,717 patients with positive and intermediate results of an intracoronary ergonovine provocation test in the VA in Korea registry (n=2,960) were classified into 100 mg/day aspirin intake (aspirin, n=743) and no-aspirin intake (control, n=974) groups. The primary end-point was a composite of major adverse cardiac events (MACEs) including cardiac death, new-onset arrhythmia, and acute coronary syndrome.
Results
The median follow-up duration was 2.0 years (25–75th, interquartile range 0.9–3.0 years). Cumulative composite MACE in the propensity score matched-pair cohort (n=1,028) was 3.6%. There was no significant difference in composite MACE between the aspirin and control groups (3.1% vs. 4.1%; hazard ratio [HR], 1.18; 95% confidence interval [CI], 0.61–2.26; p=0.623). A sensitivity analysis of only the VA-positive population showed these results to be consistent. Even for patients with minimal organic stenosis (n=369), aspirin usage was not related to the incidence of a composite MACE (HR, 1.61; 95% CI, 0.55–4.72; p=0.380).
Conclusions
Low-dose aspirin does not protect against future cardiovascular events in VA patients, even patients who combine with minimal coronary artery stenosis.
INTRODUCTION
Aspirin (acetylsalicylic acid) plays an important role in secondary prevention for patients with acute coronary syndrome (ACS).1) Nonetheless, the routine use of aspirin in the general population for the primary prevention of cardiovascular disease remains controversial as aspirin increases the risk of serious bleeding complications and exhibits insufficient efficacy.2-4) Recently, large trials such as ASPREE, ARRIVE, and ASCEND studies have reported that aspirin had no benefit for primary prevention in the general population.5-7) However, the prophylactic effect of aspirin for vasospastic angina (VA) has not yet been clearly established. Nonetheless, low-dose aspirin has been used clinically for patients with coronary artery vasospasm as a prophylactic agent regardless of the presence of coronary artery organic stenosis based on the decision of the clinician.
A prior study showed that coronary artery spasm is aggravated by high-dose aspirin.8) However, the efficacy of low-dose aspirin usage in VA remains controversial. Low-dose aspirin is thought to play a role in improving the prognosis of VA patients. Aspirin may prevent the occurrence of coronary artery spasm by limiting the production of thromboxane A2 and prostaglandin and reducing endothelial dysfunction of organic stenosis lesions.9-11) A recent study demonstrated that over 20% of VA patients showed erosion and thrombus at spasm sites defined by optical coherence tomography, suggesting the clinical use of low-dose aspirin for minimizing such endothelial injuries.12) In contrast, other recent clinical studies have suggested that low-dose aspirin not only failed to reduce cardiovascular events but could also lead to recurrent angina, contributing to rehospitalization.13-15) However, these studies have several limitations, such as being single-center retrospective observational studies or including relatively small populations.
Our study aimed to assess the 2-year clinical prognosis of low-dose aspirin usage in VA patients in a large population through a multicenter prospective observational registry.
METHODS
Study population
Between May 2010 and July 2015, a total of 2,960 patients were enrolled in the VA in Korea registry, which was designed to evaluate real-world outcomes of patients with chest pain who underwent coronary angiogram (CAG) and intracoronary ergonovine provocation tests. This large, observational registry included clinical, angiographic and 2-year long-term outcomes of patients with VA. Eleven major cardiac centers in South Korea were involved. Intermediate and significant stenosis patients (≥50% luminal diameter narrowing) were excluded from the registry. Patients with renal failure on continuous dialysis, known malignant or inflammatory diseases, or catheter-induced spasm upon baseline CAG were also excluded. All patients who showed positive results on their provocation tests or defined spontaneous spasms received medical treatments including calcium channel blockers (CCBs) and other vasodilators during the follow-up. Medications for non-positive subjects were prescribed based on the clinician's decision. More information on the baseline population of this registry can be found in our recently reported article.16)
CAG and provocation test: definitions of positive and intermediate results
We confirmed that none of the patients took a VA drug within at least 48 hours of the tests. After coronary angiography from right coronary artery to left coronary artery, intracoronary ergonovine infusion was performed, as described previously.16) After induced spasm, nitrate was infused and recovery of coronary artery dilation was confirmed. VA was diagnosed according to the guidelines for diagnosis and treatment of patients with VA of the Japanese Circulation Society.17) A positive diagnosis included spontaneous vasospasm (>90% luminal diameter narrowing), presence of total or subtotal (>90%) ischemic symptoms and/or electrocardiography (ECG) changes. A negative diagnosis included <50% luminal narrowing without symptoms or ECG change. The other cases are diagnosed as an intermediate result and reclassified to possible VA or probable VA. A possible intermediate result included a case of total or subtotal luminal narrowing (>90%) without ischemic symptom and ECG changes or 50–90% luminal narrowing with or without symptom. A probable intermediate result included 50–90% luminal narrowing without ischemic symptom or ECG changes. All vascular responses to ergonovine in the provocation test and atherosclerosis on baseline CAG were quantitatively analyzed for epicardial coronary artery diameters≥2.5 mm by clinicians unaware of patient status at the core laboratory of Seoul St. Mary's Hospital, Seoul, South Korea.
Definition and primary outcome
An ischemic ECG change was defined as an ST-segment elevation or depression >0.1 mV or a negative U-wave recorded from at least 2 related leads. Cardiac death was defined as any death due to a proximate cardiac cause such as myocardial infarction (MI), low-output failure, fatal arrhythmia, or death from unknown causes. Patients who presented clinically significant arrhythmia, including atrial or ventricular tachycardia/fibrillation, symptomatic premature beats, sick-sinus rhythm, or atrioventricular block for the first time during the follow-up were considered to have the new-onset arrhythmia.18) ECGs were routinely evaluated during the regular or emergency visits, and 24-hour Holter monitoring was also performed in patients with suspicious symptoms. The primary outcome was the 2-year incidence of major adverse cardiac events (MACEs) composed of cardiac death, new-onset arrhythmia, and ACS.
Follow-up
Each patient was followed up at out-patient clinics or by telephone questionnaire annually. Information regarding patient death was obtained from hospital records or from the guardians of the patients via telephone. All clinical outcomes of interest were confirmed by source documents and were centrally adjudicated by a local events committee and by an independent group of clinicians who were unaware of patient status. Information regarding death was matched with records from the National Population Registry of the Korea National Statistical Office with a unique personal identification number to validate mortality follow-up data. The study protocol was approved by the ethics committee at each participating center. Written informed consent was obtained from all participants.
Statistical analysis
Continuous variables are summarized as the mean±standard deviation, and categorical variables are summarized as the number (%). Differences between groups were analyzed using the Student's t-test or Welch's t-test for continuous variables and χ2 test or Fisher's exact test for categorical variables. Cumulative incidence rates were estimated by the Kaplan-Meier method and compared using the log-rank test. Cox proportional hazard models were applied to analyze hazard ratios (HRs) of risk factors for endpoints and 95% confidence intervals (CIs). Propensity scores (PSs) were estimated with multivariate logistic regression models. The data were matched using a greedy nearest neighbor matching method with individual PSs and were considered with a caliper width of 0.20.19) In the PS-matched population, continuous variables were analyzed using a paired t-test, and categorical variables were analyzed by McNemar's test. Statistical analyses were performed with SAS 9.4 (SAS Institute, Cary, NC, USA). All tests were 2 tailed, and p<0.05 was considered significant.
RESULTS
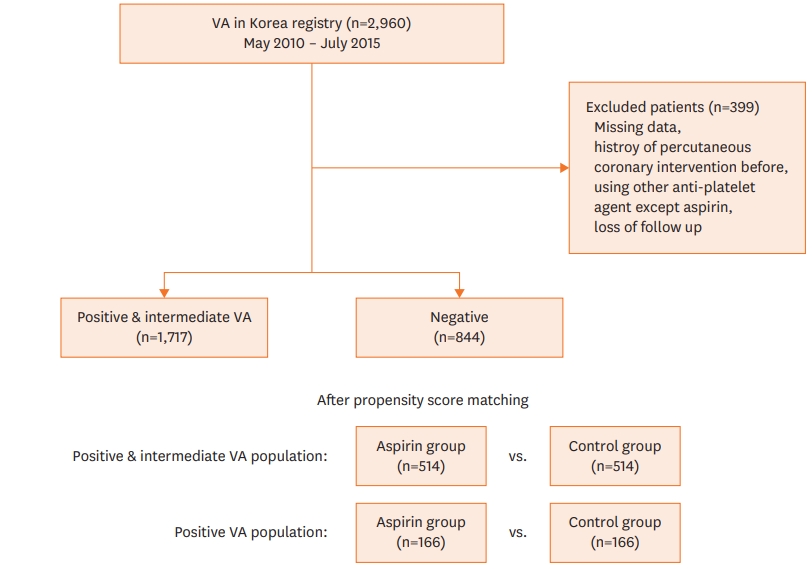
Patient enrollment and incidence
Of the 2,960 patients who presented chest pain and underwent CAG, the final diagnosis information of 95 patients was missing, 47 patients had a history of prior percutaneous coronary intervention, 111 patients used anti-platelet agents other than aspirin, and 146 patients were lost to follow-up; these patients were excluded from the study analysis. Thus, a total of 2,561 patients with suspected VA were enrolled. We divided the total patients into a positive and intermediate population (total, n=1,717; 617 & 1,100, each) and a negative population (n=844) according to the outcome of the ergonovine provocation test. Patients in the positive and intermediate populations were reclassified into a low-dose aspirin (100 mg once daily) intake (aspirin, n=743) group and a no-aspirin intake (control, n=974) group to evaluate long-term clinical implications of low-dose aspirin in VA. The median followup duration was 2.0 years (25–75th, interquartile range [IQR], 0.9–3.0 years). The 2-year incidences of MACE (cardiac death, new-onset arrhythmia, and ACS) were determined. The patients had normal findings (n=1,067) or minimal (<50% luminal diameter narrowing) atherosclerosis upon baseline CAG in the positive and intermediate group, as shown in the study outline (Figure 1).
Baseline characteristics
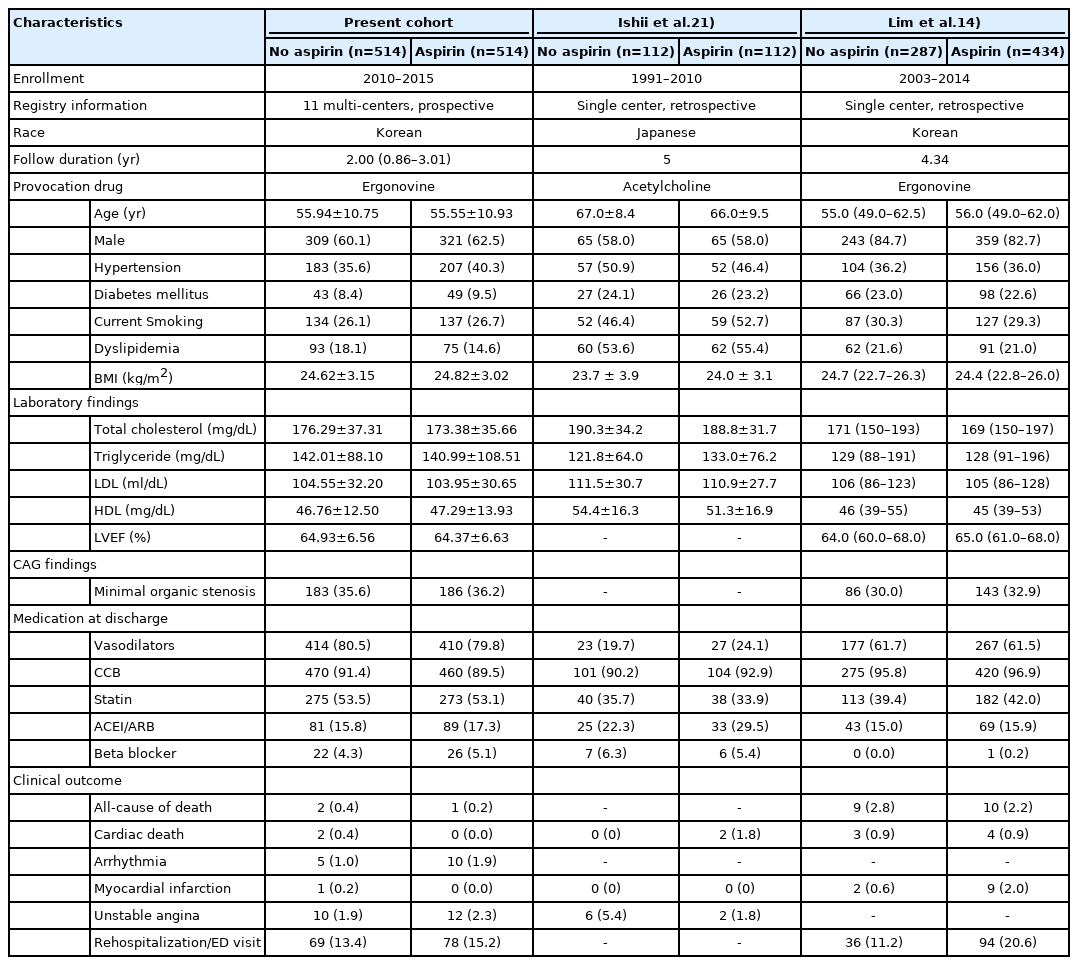
In the unmatched positive and intermediate group (n=1,717), the mean age in the aspirin group was 56.94±11.05 years, which was significantly higher than that of the control group (Table 1). However, only 20% of patients were aged ≥65. In the aspirin group, patients were significantly older and had significantly higher rates of hypertension, diabetes, tachyarrhythmia history, being female and currently smoking. Meanwhile, patients who showed organic minimal stenosis on CAG used more aspirin (p<0.001). Upon discharge, the use of nicorandil, statin and angiotensin receptor blocker/angiotensin converting enzyme inhibitor were used significantly more in the aspirin group (p<0.001). Approximately 90% of patients were prescribed CCBs as discharge medicine. The usage of beta blockers was very low, corresponding to approximately 6% of patients in both groups, and most patients in the intermediate group were previously prescribed medicine for hypertension. PS matching was applied to adjust for differences in the baseline characteristics of both groups, yielding a total of 1,028 patients: 514 patients using aspirin and 514 patients not using aspirin. After PS matching, the baseline characteristics were similar between the 2 groups. All standardized differences were below 10%, as described in Table 1.
Clinical outcomes of the overall population
The cumulative composite MACE in the total positive and intermediate VA group was 3.6%. The Kaplan-Meier curves for the primary outcome was not significantly different between groups, corresponding to 3.1% vs. 4.1% for the aspirin group versus the control group (HR, 1.18; 95% CI, 0.61–2.26; p=0.623). The rate of cardiac death was very low at approximately 0.17%. Cardiac death occurred only in the positive group. The prevalence rates of new-onset arrhythmia and ACS were low in the crude population (2.0% vs. 0.9%; p=0.056; 3.0% vs. 2.6%, p=0.620, respectively). Only new-onset atrial fibrillation occurred significantly more in the aspirin group (0.9% vs. 0.2%, p=0.045).
Clinical outcomes of the PS-matched group analysis
PS matching yielded 514 pairs with more balanced baseline characteristics (Table 1). Cumulative composite MACE in the PS-matched cohort was 3.6% over a median follow-up duration of 2.0 years (25–75th, IQR, 0.9–3.0 years). The prevalence of cardiac death, new-onset arrhythmia, ACS, stroke and rehospitalization was 0.2%, 1.5%, 2.2%, 0.2%, and 14.3%, respectively (Table 2). Low-dose aspirin treatment was not associated with increased composite MACE (4.1% vs. 3.1%, log-rank p=0.623). The Kaplan-Meier curves demonstrated no significant difference between the 2 groups, as shown in Figure 2A. Cardiac death rate was too low to evaluate the treatment effect during the 2-year follow-up period (aspirin vs. control group, 0% vs. 0.4%, log-rank p=0.492) (Figure 2B). The incidence of new-onset arrhythmia and ACS showed no differences between the control and low-dose aspirin treatment groups (1.9% vs. 1.0%, log-rank p=0.260; 2.3% vs. 2.1%, log-rank p=0.900, respectively) (Figure 2C-D). Rehospitalization or emergency department visits was also similar in both groups (15.2% vs. 13.4%, log-rank p=0.909). Even for patients with minimal organic stenosis (n=369), aspirin usage was not related to the incidence of composite MACE (HR, 1.61; 95% CI, 0.55–4.72; p=0.384).
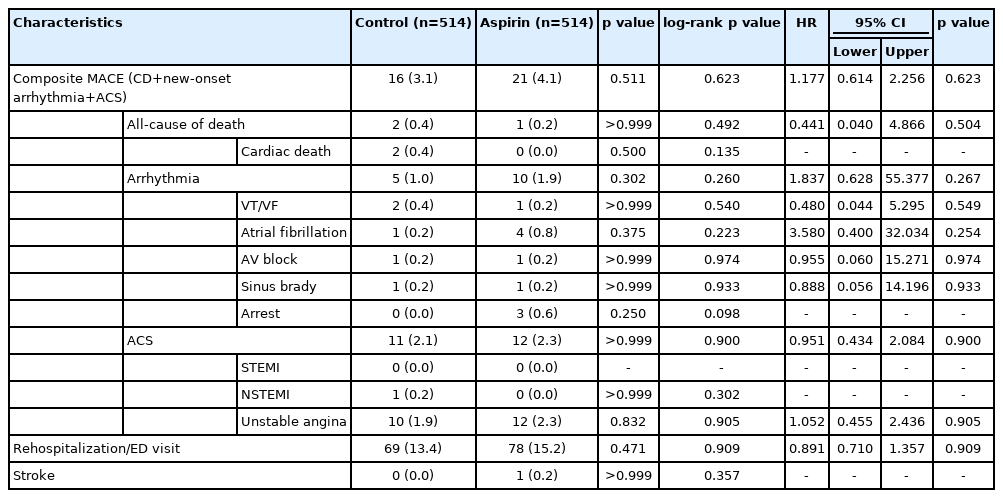
Cumulative outcomes and Cox proportional hazard ratios according to aspirin treatment among propensity-matched patients in the positive and intermediate VA populations
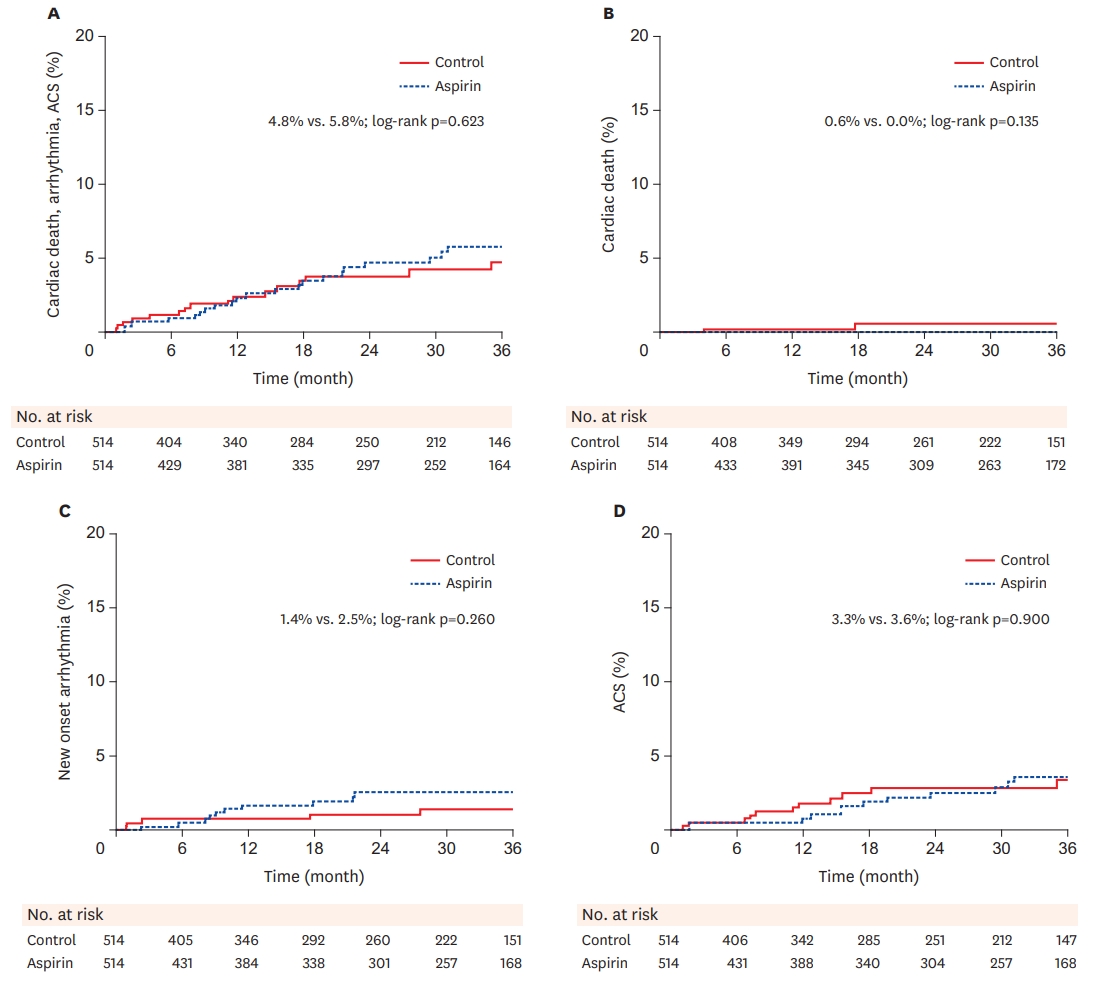
Kaplan-Meier incidence curves of outcomes in 514 propensity-matched pairs in the positive and intermediate vasospastic angina groups. Long-term incidences in the 2 groups are presented as percentages and were statistically compared with the log-rank test. (A) Incidences of composite major adverse cardiac event, (B) Incidences of cardiac death, (C) Incidences of arrhythmia, (D) Incidences of acute coronary syndrome.
ACS = acute coronary syndrome.
Cox regression hazards analysis of composite MACE in PS-matched patients
According to the unadjusted Cox regression analysis, an age over 65, male sex, hypertension, diabetes, currently smoking, alcohol, LDL ≥160, presence of minimal organic stenosis and myocardial bridge on baseline CAG, and vasodilator, CCB, statin, and beta blocker usage were not independent predictors for the primary end-point during the 2 years. Data were adjusted for possible confounding variables, including previously known conventional risk factors.20) Only creatinine was a significant independent predictor of a higher risk of composite MACE.
Subgroup analysis among PS-matched patients
Regarding the prespecified subgroup analysis, MACE interaction analysis showed that the association of aspirin usage with MACE was not modified by age over 65, gender, hypertension, diabetes mellitus, smoking, hyperlipidemia, left ventricle ejection fraction, the presence of organic minimal stenosis on baseline CAG, statin, vasodilator and beta blocker usage (p>0.01 for each, Figure 3).
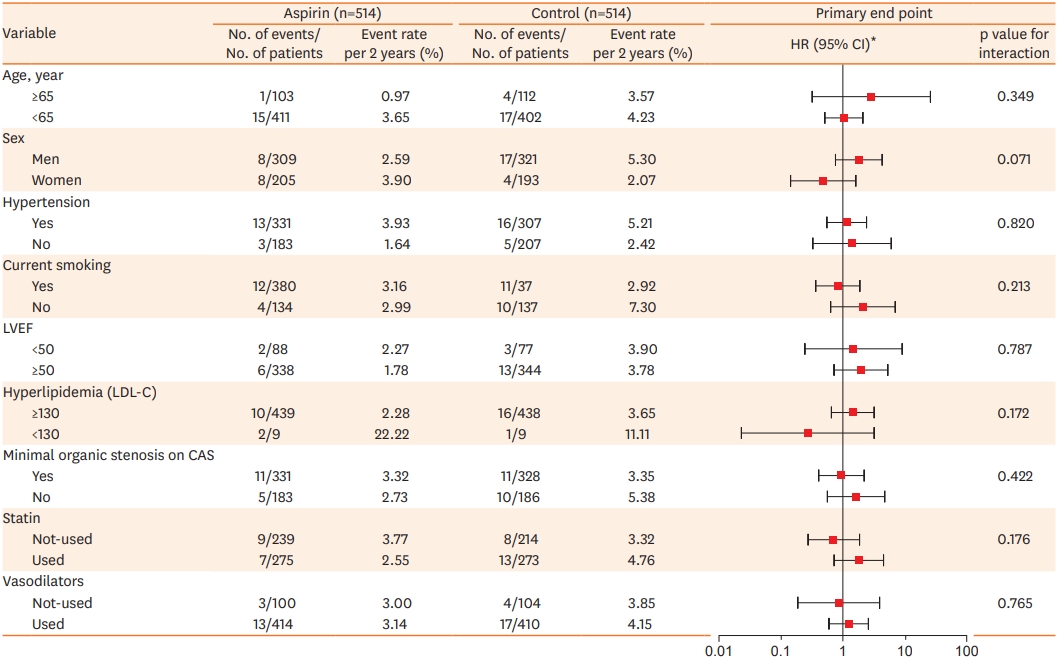
HR for aspirin vs. control group and event rates for the primary composite outcome among propensity-matched patient. CAG = coronary angiogram; CI = confidence interval; HR = hazard ratio; LAS = low dose aspirin; LDL-C = Low-density lipoprotein Cholesterol; LVEF = left ventricle ejection fraction.
*HRs are for the LAS group, as compared control group.
Sensitivity analysis of a VA-positive population
We conducted a sensitivity analysis on a completely VA-positive population because the intermediate group is not definitively diagnosed as VA according to the Guidelines of the Japanese Circulation Society, which could bias the results.17) Upon matching PSs, we generated 166 pairs of patients between the aspirin and control groups. Low-dose aspirin treatment was not associated with increased composite MACE (7.2% vs. 4.2%; log-rank p=0.440). The Kaplan-Meier curves also showed no significant difference between the 2 groups.
DISCUSSION
In this multi-center prospective registry study, 100 mg/day aspirin was prescribed to 749 of 1,717 VA patients (43.6%). The decision to treat was made by the physician based on older age, hypertension, diabetes, and minimal organic stenosis on CAG. After PS matching analysis, low-dose aspirin showed a neutral effect in preventing future cardiac events in VA patients during a 2-year follow-up period. Moreover, there was no significant difference between the 2 groups regarding the incidence of unstable angina or rehospitalization. The presence of minimal organic stenosis in coronary artery was not related to adverse outcomes.
Based on previously revealed mechanisms, aspirin is thought to reduce adverse cardiac events and is thus prescribed to VA patients as a prophylactic agent. It has been suggested that aspirin may prevent the initiation of VA and prevent thrombus formation caused by repetitive spasm. However, high doses of aspirin have been reported to aggravate coronary artery spasm;8) the acetylation of cyclooxygenases alters the enzyme that produces aspirin-triggered lipoxin and it inhibits thromboxane A2 and prostaglandin production.9) Low-dose aspirin is expected to mainly exert its effect not by inhibiting prostacyclin but by suppressing thromboxane A2, and it may reduce vasoconstriction, resulting in less coronary artery spasm.
Recent studies, including ours, demonstrate that low-dose aspirin does not reduce future cardiovascular events such as cardiac death and MI in VA patients, regardless of concomitant insignificant coronary artery stenosis (Table 3).14)21) However, contradictory results regarding the incidence of recurrent ischemic chest pain have been reported. Ishii et al. demonstrated that a lower incidence of unstable angina occurred in a group taking aspirin.21) In contrast, Lim et al. reported that those taking aspirin showed a higher tendency for recurrent angina contributing to rehospitalization.14) In this study, the aspirin group had much minimal organic stenosis, which might result in a higher incidence of rehospitalization due to angina (Table 3). In addition, both studies were limited by their single-center retrospective nature. Our multi-center prospective data demonstrate that low-dose aspirin has a neutral effect on reducing rehospitalization or emergency department visits due to recurrent angina (Table 3).
VA-KOREA results in the context of similar clinical trials in different patient populations with variant angina
The benefits of low-dose aspirin for the general population as primary prevention are less clear because cardiovascular risk is lower when considering primary prevention compared to secondary prevention, whereas the bleeding risk is similar.3)5)22)23) Therefore, physicians should consider the individual patient risk/benefit ratio in deciding whether to use aspirin for primary prevention. A recent study classified patients into “aspirin recommend,” “uncertainty area,” and “aspirin not recommend” groups by suggesting a threshold risk level of aspirin. They proposed such a threshold as a risk of major cardiovascular events (death, MI and stroke) of ≥2 per 100 patient-years and <1.0 per 100 patient-years.24) The threshold risk level of 2 major cardiac events/100 patient-years corresponds approximately to 7% to 10% of traditional 10-year CVD risk.25-27) In our study, death, MI and stroke risk of VA patients after usage of low-dose aspirin were 0.3, 0.1 and 0.2 per 100 patient-years, respectively. Hence, we can categorize the VA population into the “aspirin not recommend” group.
The association between VA and the progression of coronary atherosclerosis lesion remains unclear. Prior studies have demonstrated that coronary spasm plays a potential role in atherosclerosis progression and frequently occurs at the site of significant organic stenosis.28)29) To reduce the confounding bias, we excluded patients who had intermediate and significant stenosis lesions on baseline CAG and patients with a prior history of percutaneous coronary intervention. In our subgroup study, the association between the usage of aspirin and composite MACE was not modified by the presence of minimal organic stenosis on baseline CAG. (HR, 1.03; 95% CI, 0.41–2.60; p=0.955).
Compared to previous reports, the strengths of this study include the large cohort size based on a registry comprising eleven centers and the well distributed data using the PS matching method. Low-dose aspirin usage did not show a protective effect for cardiac mortality, newonset arrhythmia, or ACS occurrence in the positive and intermediate VA groups. Aspirin also did not lower the occurrence of combined MACE and rehospitalization. We suggest that aspirin is not needed for the primary prevention of CVD in VA patients.
This study has several limitations. Our study was a prospective observational multicenter registry study with a retrospective design. Entry into the registry may not be as strictly monitored compared with randomized control trials, and the follow-up periods varied across individual patients. Second, we could not analyze safety issues due to lack of complication data such as bleeding. Finally, the adverse events in our study were too low to establish the outcome despite that the mean follow-up duration was 2 years. To clarify the long-term effects of aspirin usage in VA, longer follow-up data are needed. More studies are required to evaluate the efficacy and safety of aspirin in VA patients, including randomized control trials and long-term follow-up data.
In conclusion, low-dose aspirin did not protect against future cardiovascular events in VA patients with intracoronary ergonovine provocation regardless of the presence of minimal coronary artery stenosis during 2 years.
Notes
Conflict of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Shin DI, Baek SH; Data curation: Shin DI, Kim DS, Choi DJ; Formal analysis: Her SH, Myong JP; Investigation: Han SH, Rha SW, Jo SH; Methodology: Lim SC; Resources: Ahn Y, Kwon HM; Supervision: Ahn Y, Gwon HC; Writing - original draft: Lee KY; Writing - review & editing: Lee KY, Baek SH.