Public awareness of cardiovascular disease prevention in Korea
Article information
Abstract
Background
The burden of cardiovascular disease (CVD) is significant in Korea. Ultimately, public knowledge and awareness of CVD risk factors and prevention are essential to reduce its burden. Hence, this study aimed to examine the level of public awareness of CVD risk factors and prevention in Korea in 2022.
Methods
We used data from the Cardiovascular Disease Prevention Awareness Survey conducted by the Korean Society of Cardiovascular Disease Prevention in June 2022. Using a structured web-based questionnaire, 2,000 individuals aged 20 years or more were surveyed on computers or mobile devices. Information on sociodemographic characteristics, the presence of cardiometabolic disease, CVD concerns and self-assessed likelihood, and awareness of CVD prevention were analyzed.
Results
Cancer (44.3%) was the most feared disease, followed by CVD (19.5%). Nevertheless, most respondents stated that they were likely to develop CVD in their lifetime (67.4%). Only 9.2% of respondents were aware of the details of recommendations to prevent CVD, and this level of knowledge was also low among respondents with cardiometabolic diseases (10.7%). Not smoking, being physically active, eating a healthy diet, and reducing alcohol consumption were deemed easy to implement. On the contrary, reducing stress, being physically active, and eating a healthy diet were considered the most difficult recommendations to practice.
Conclusions
Public awareness of CVD risk factors and prevention appeared to be insufficient in Korea. Our research suggests that simple but practical recommendations should be conveyed and promoted to raise public awareness, which is currently inadequate.
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death and disability worldwide [1]. In previous decades, considerable global efforts have achieved substantial progress in reducing CVD mortality rates [2]. However, population aging has canceled out these improvements; the absolute number of CVD cases doubled from 271 million in 1990 to 523 million in 2019, while that of deaths increased from 12.1 million to 18.6 million [2,3]. Korea has also been challenged by mortality and morbidity from CVD. Specifically, stroke and ischemic heart diseases account for the highest number of deaths following cancer in Korea [4].
According to the World Health Organization, more than 75% of CVD development can be prevented by reducing risk factors [5,6]. Numerous institutes, organizations, and governments have distributed guidelines and recommendations for health professionals, clinical practitioners, and the public; examples include the European Society of Cardiology Guideline, the American College of Cardiology and American Heart Association Guideline, and simplified recommendations such as Life’s Simple 7 [7–10]. Likewise, the health sector of the Korean government has been concerned about increasing rates of CVD and promoted recommendations to prevent CVD [11]. The goals of these recommendations, however, appear to be only partly accomplished. Previous studies illustrated that unmodified but prevalent risk factors—in particular, physical activity and obesity—increased the occurrence of CVD in Korea along with rapid population aging [5,6]. For the successful implementation of risk modification, individuals need to be well-acquainted with the possible risks of CVD determinants and how to mitigate them [12,13]. However, studies or surveys on the public awareness of CVD in Korea have been rather insufficient compared to those on cancer, the awareness of which is monitored biannually by the National Cancer Center Prevention Awareness Survey.
To evaluate the levels of public knowledge and perceptions of CVD, the Korean Society of Cardiovascular Disease Prevention (KSCP) conducted a survey in 2022. This study aimed to report the level of public awareness of CVD and CVD prevention based on this survey, thereby identifying the most necessary and urgent targets for CVD prevention.
METHODS
Data source
We analyzed the results from the Cardiovascular Disease Prevention Awareness Survey conducted by KSCP in 2022. The survey, which was carried out by a professional research agency, collected data from individuals aged 20 years or more across Korea. It employed a stratified sampling design based on age and sex. A structured web-based questionnaire was sent and filled out on computers or mobile devices. In total, 2,000 individuals aged between 20 and 69 years responded across the 17 provinces of Korea in June 2022.
Questionnaires and variables
The structured questionnaire in the survey was designed to investigate five factors comprising 31 items: sociodemographic characteristics (8 items), the presence of cardiometabolic disease (1 item), CVD concern and self-assessed CVD likelihood (4 items), awareness and practice of CVD prevention (12 items), and changes in health behaviors after COVID-19 (6 items).
Sociodemographic information included age, sex, marital status (single, married, bereaved/separated/divorced), monthly household income (less than 3 million, 3 to 6 million, more than 6 million KRW), and educational attainment (middle school or less, high school, college or more). Respondents were asked about the presence of cardiometabolic diseases, which were defined as being diagnosed with CVD (coronary heart disease and cerebrovascular disease) or CVD-related diseases (hypertension, diabetes, and dyslipidemia).
The levels of individuals’ concerns about and self-assessed likelihood for CVD were measured in comparison with other diseases known to cause high mortality or disability-adjusted life years (DALYs) based on the Korean Burden of Disease Study: cancer, musculoskeletal diseases, dementia, and psychiatric disorders [14,15]. Respondents were also asked how likely they were to have CVD someday on a 5-point scale. Those who responded “likely” and “very likely” were asked a follow-up question about the reason for their response.
In terms of CVD prevention, respondents were comprehensively asked how familiar they were with CVD prevention recommendations, with three response options (not having heard of CVD prevention recommendations, having heard of them but not knowing any details, and knowing details about how to prevent CVD). To evaluate public knowledge and practice for each CVD risk factor, the guideline for CVD prevention published by the Korea Disease Control and Prevention Agency was used [11]. This guideline includes nine recommendations: (1) do not smoke; (2) drink no more than one or two drinks per day; (3) eat a healthy diet such as unsalted and nutritionally balanced food; (4) engage in moderate exercise for at least 30 minutes every day; (5) keep an appropriate body weight and waist circumference; (6) reduce stress and improve mental health; (7) regularly check blood pressure, blood sugar, and cholesterol and manage them; (8) treat hypertension, diabetes, and dyslipidemia; and (9) be aware of the emergency symptoms of stroke and myocardial infarction, and go to the hospital immediately if symptoms occur [11]. For these nine rules, respondents were asked to assess their importance for preventing CVD, and to choose the most and the second most easy or difficult item to practice.
Statistical analyses
Our study mainly used descriptive analyses such as frequency and proportions. Since the prevalence of awareness is expected to be different according to the presence of CVD, subgroup analyses were conducted after analyzing the total study sample. For respondents’ general characteristics and all items related to awareness of CVD, comparisons between respondents with cardiometabolic disease and those without used the t-test and chi-square test. To identify the most vulnerable populations in terms of CVD prevention, we used univariate logistic models. In these models, the following possible risk factors were included as independent variables: age (10-year groups), sex, marital status, education, monthly household income, and the presence of cardiometabolic disease. All analyses were carried out using SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Respondents’ characteristics
Table 1 shows the survey respondents’ sociodemographic characteristics and the presence of diagnosed cardiometabolic disease. Dyslipidemia and hypertension were the most prevalent conditions in our study, reported by 22.1% and 19.4% of respondents, respectively. Respondents with cardiometabolic disease were more likely to be older, male, married, and in the middle-income bracket.
Concern about and the likelihood of CVD
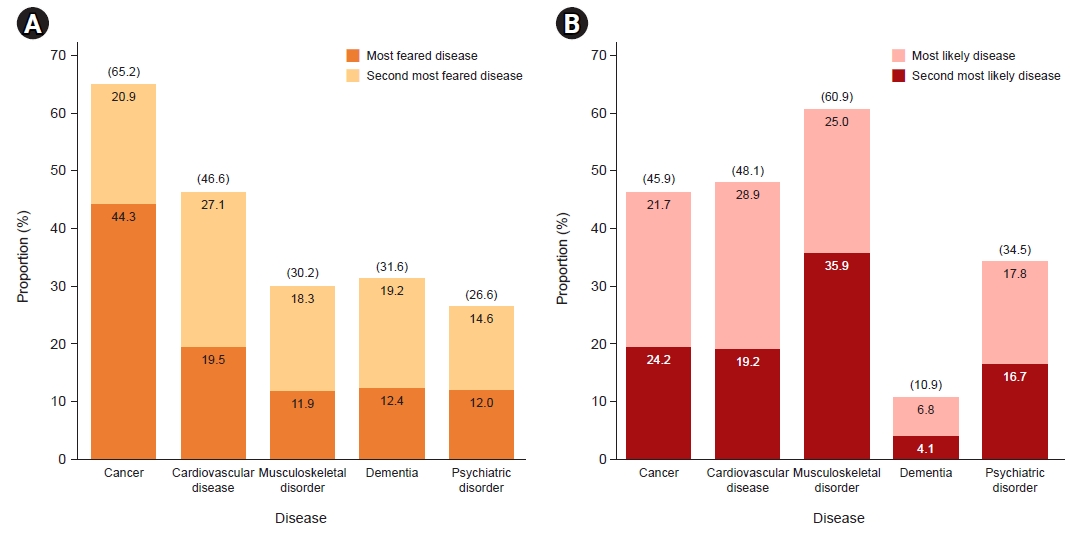
Among the five diseases that respondents were asked about, cancer (65.2%) was the most feared, followed by cardiovascular disease (46.6%) (Fig. 1A, Table S1). According to the respondents’ self-assessments, the disease that they would most likely experience within 10 years was musculoskeletal disorders, such as back pain and arthritis (60.9%), followed by CVD (48.1%) (Fig. 1B, Table S1). When stratified by the presence of cardiometabolic diseases, even those with those diseases feared cancer more than CVD (Table S2). Logistic regression models showed that older age, male sex, being married, higher household income, and the presence of a cardiometabolic disease were significantly associated with both CVD concern and self-assessed likelihood of developing CVD (Table S3). When questioned about how likely they were to develop CVD in the future, 67.4% of respondents answered “likely,” 21.9% “neutral,” and 10.8% “not likely” (Fig. S1A). Regardless of the presence of a cardiometabolic disease, the reasons for which they rated their CVD likelihood as high were unhealthy behaviors, family medical history, and not being able to afford to take care of their health (Fig. S1B).
Awareness of CVD prevention
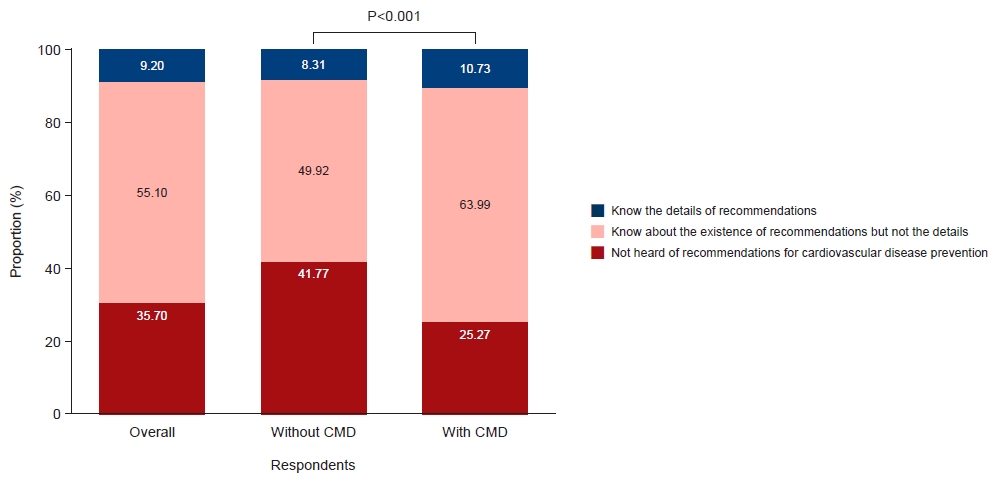
Over half of respondents (55.1%) were aware that there were recommendations for CVD prevention but did not know the details. A considerable proportion (35.7%) had never heard of recommendations, and only a few (9.2%) knew the details of healthy behaviors that hinder CVD development (Fig. 2). Respondents with cardiometabolic diseases were more likely to be aware of the existence of recommendations. However, their knowledge of the details was only slightly higher (10.7%) than those without diseases (8.3%) (Fig. 2). In a logistic regression model, sociodemographic factors were not significantly associated with the awareness of recommendations for CVD prevention (Table S4).
Based on the nine recommendations for CVD prevention promoted by the government program for the prevention and management of cardiocerebrovascular diseases, the public awareness of each recommendation was investigated (Fig. 3). Across all recommendations, over 80% of respondents agreed on their importance to prevent disease. In particular, not smoking, a timely intervention when the symptoms of myocardial infarction or stroke occur, and being physically active were considered critical. In contrast, the importance of managing biometric measures (blood pressure, blood sugar, and cholesterol), and drinking less were rated relatively low.
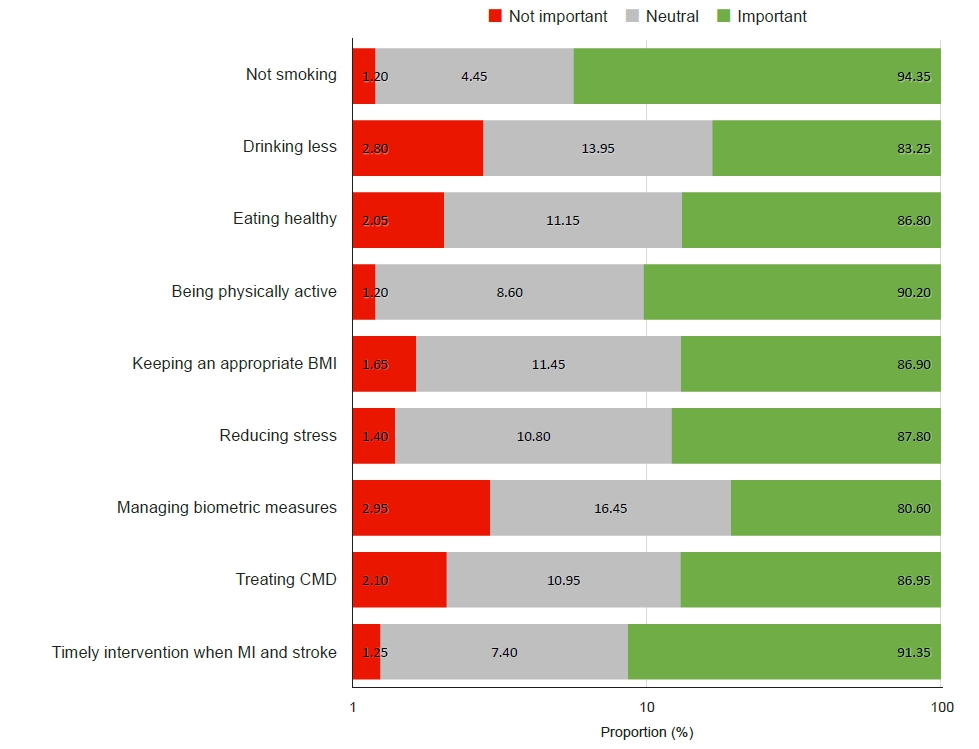
Perceived importance of each recommendation for cardiovascular disease prevention. BMI, body mass index; CMD, cardiometabolic disease; MI, myocardial infarction.
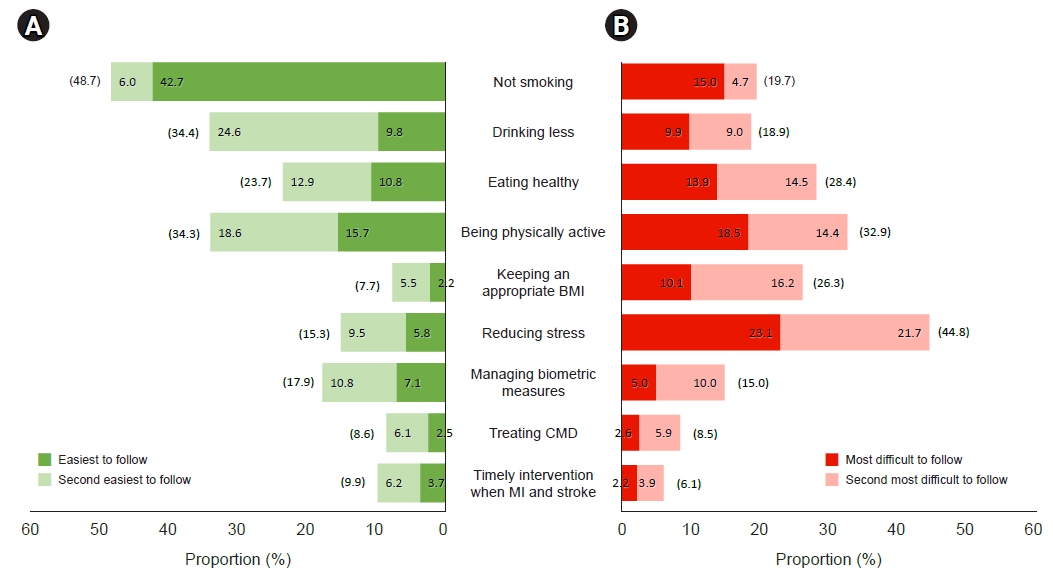
Of the nine recommendations, not smoking (42.7% as the easiest item, 6.0% as the second easiest item), engaging in daily exercise for at least 30 minutes (15.7% as the easiest item, 18.6% as the second easiest item), eating a healthy diet (10.8% as the easiest item, 12.9% as the second easiest item), and reducing alcohol consumption (9.8% as the easiest item, 24.6% as the second easiest item) were deemed relatively easy to implement (Fig. 4A). On the contrary, people had difficulties in reducing stress (23.1% as the most difficult item, 21.7% as the second most difficult item), engaging in daily exercise for at least 30 minutes (18.5% as the most difficult item, 14.4% as the second most difficult item), and eating a healthy diet (13.9% as the most difficult item, 14.5% as the second most difficult item) (Fig. 4B). These findings were not significantly different according to the presence of a cardiometabolic disease (Table S5).
DISCUSSION
Overall, public awareness of CVD risks and prevention appeared to be insufficient among Korean adults. CVD was rated as the second most worrisome and the second most likely disease in comparison with cancer, musculoskeletal disorders, dementia, and psychiatric disorders. Older age, male sex, being married, higher household income, and presence of cardiometabolic disease were significantly associated with CVD concern and self-assessed likelihood. Furthermore, too few respondents were aware of the details of CVD recommendations, although people recognized their importance for prevention.
Among the diseases that cause a public health burden in Korea, cancer was the most feared. Even people with cardiometabolic disease feared cancer more than CVD, most likely because they were familiar with the high mortality from cancer. In a study on the burden of disease in Korea from 2000 to 2010, the DALYs per 100,000 for cancer were on the rise and ranked first [16]. Ischemic heart disease and cerebrovascular disease also constituted a large portion of the disease burden. In particular, the DALYs due to ischemic heart disease were comparable to those of cancer in 2010 [16].
When questioned about the likelihood of developing CVD in their lifetime, 67.4% of respondents agreed on its possibility. This might imply a vague public perception of CVD risk, considering CVD as a possible disease in later life, rather than an imminent threat. Such an interpretation is consistent with a high odds ratio for agreement of CVD likelihood among respondents in their 50s (adjusted odds ratio, 2.56; 95% confidence interval, 1.79–3.68), compared to respondents in their 20s. In addition, male sex, married status, and higher household income were associated with higher anxiety and self-assessed likelihood of CVD.
Despite high concerns about CVD, few respondents were aware of the details of the recommendations for CVD prevention. Even among respondents with cardiometabolic disease, who should be most informed, only 10.7% of individuals were familiar with the details. Other studies have also reported a lower awareness of detailed information than of the existence of guidelines. A qualitative study of a cervical cancer awareness survey among female college students in Korea pointed out that the existence of the vaccination campaign itself is known through various media and channels, but those measures have been insufficient to convey specific details [17]. It will be necessary to improve the delivery of health information. Previous research has also reported varying effects of information delivery channels. A study on the effective promotion of regular health check-ups showed that health information delivery via television programs was most effective in inducing behavioral changes and disseminating information [18]. To promote healthy behaviors for CVD prevention, a detailed and effective information delivery system should be discussed and implemented.
In our study, not smoking, being physically active, eating a healthy diet, and reducing drinking were selected as the easiest recommendations to follow. However, stress management was pointed out as the most difficult recommendation to carry out. An association between stress and CVD has been demonstrated in previous studies. Stress activates inflammation and coagulatory mechanisms, causes CVD incidence (e.g., myocardial infarction), and increases CVD event recurrence and mortality [19]. A Korean study found that high stress was significantly associated with the prevalence of CVD, especially in men (adjusted odds ratio, 2.31; 95% confidence interval, 1.28–4.17) [20]. Stress management interventions can reduce CVD risk and might improve the quality of life among CVD patients [21]. It is also notable that a considerable number of people thought that being physically active and eating healthy were the easiest recommendations to follow, while many answered that they were the most difficult. This implies that tailored strategies for lifestyle modification should be established.
Public awareness of cancer has been regularly monitored in Korea [22,23], but awareness of CVD has been less frequently investigated. Our study was the first—at least, in a long time—to examine public awareness of CVD in Korea. Nevertheless, several limitations should also be taken into consideration. First, although the Cardiovascular Disease Prevention Awareness Survey was conducted throughout the nation, the sample size was not sufficient to compare subgroups according to sociodemographic factors such as income, education, and region. Second, although the survey made efforts to obtain as much objective data as possible (e.g., by measuring the level of CVD awareness by comparison with other diseases), the questionnaire was self-reported, and items were subjectively rated. Last, there might have been differences in characteristics and awareness between respondents and nonrespondents. The survey was conducted on computers or mobile devices, which might have led to different response rates according to familiarity with electronic devices.
Examining public awareness of CVD risks and prevention is critical to formulating the most necessary and urgent strategies for CVD prevention. Our research suggests that simple but practical recommendations should be discussed and actively pursued in order to raise insufficient public awareness. In particular, health authorities and policymakers must encourage people to develop healthy behaviors that they have found difficult to practice, such as managing stress, regularly engaging in moderate exercise, and eating a healthy diet.
Supplementary Material
Table S1. The most feared and the most likely disease (n=2,000)
cpp-2022-4-e20-suppl1.pdfTable S2. The most feared and the most likely disease according to the presence of cardiometabolic diseases (n=2,000)
cpp-2022-4-e20-suppl2.pdfTable S3. The risks that CVD was selected as the most feared and the most likely disease according to socioeconomic factors
cpp-2022-4-e20-suppl3.pdfTable S4. Odds ratio of awareness of recommendations according to socioeconomic factors
cpp-2022-4-e20-suppl4.pdfTable S5. The easiest and the most difficult recommendation to follow according to the presence of CMD (n=2,000)
cpp-2022-4-e20-suppl5.pdfFig. S1. The results of (A) perceived likelihood of cardiovascular disease development in lifetime and (B) the reasons of the likelihood.
cpp-2022-4-e20-suppl6.pdfSupplementary materials are available at https://doi.org/10.36011/cpp.2022.4.e20.
Notes
Ethical statements
Not applicable.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
None.
Acknowledgments
The current study used data from the Cardiovascular Disease Prevention Awareness Survey, which was conducted by the Korean Society of Cardiovascular Disease Prevention (KSCP) and surveyed by a professional research agency (Embrain, Seoul, Korea).
Author contributions
Conceptualization: EK, CHJ, WYL; Data curation: EJR, HCK; Formal analysis: EK; Methodology: JN, HCK; Supervision: HCK; Validation: HJP, SP, WYL; Visualization: SHI, EK; Writing–original draft: EK; Writing–review & editing: CHJ, EJR, JN, JHL, HJP, SP, SHI, WYL, HCK.