Perioperative Management of Hypertensive Patients
Article information
Abstract
Due to the high prevalence of hypertension, hypertensive patients undergo perioperative evaluation and management. Severe hypertension may increase the operative risk. However, hypertension with a diastolic blood pressure of less than 110 mmHg usually does not appear to increase the risk. In general, it is recommended that oral antihypertensive drugs be continued before and after surgery. In particular, sympathetic blockers, such as beta-blockers, should be maintained. It is generally recommended to continue intake of calcium channel blockers, especially for surgeries with a low bleeding risk. However, in the case of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, it is recommended that they be stopped 24 hours before surgery because they can inhibit excessive compensatory renin-angiotensin activation during surgery. Statin and aspirin medications are often prescribed for patients with hypertension. It is recommended to continue intake of statins in the perioperative period. Aspirins are recommended for low-risk patients undergoing noncardiac surgery.
INTRODUCTION
Hypertension (HT) affects most adults and is steeply increasing in the elderly population across the globe.1)2) The prevalence of HT as an individual cardiovascular risk factor in patients aged 45 years or older undergoing non-cardiac surgery has temporally increased from 52% in 2004–2005 to 63% in 2012–2013 in the US.3)
Nearly half of all patients undergoing surgery take medications for chronic, noncommunicable diseases.4) The majority of medications are cardiovascular drugs, accounting for 48% of all drugs.4) HT is the most common comorbidity, being the reason for up to 27% of postponed surgeries.5) Frequently, hypertensive patients experience intraoperative blood pressure (BP) lability, which can lead to myocardial ischemia in the worst-case scenario.6) In a meta-analysis of 30 observational studies, HT preceding operative procedures was associated with a 35% increase in cardiovascular complications7); therefore, proper perioperative management is required.8) This review aims at summarizing perioperative risk stratification and management of hypertensive patients undergoing surgery.
PERIOPERATIVE RISK STRATIFICATION OF HYPERTENSIVE PATIENTS
During the induction of anesthesia, sympathetic nerve activation may increase BP by 20 to 30 mmHg and heart rate by 15 to 20 times per minute in normal subjects and may cause a more exaggerated response in hypertensive patients.9) The average arterial pressure decreases with the passage of anesthesia time, and BP and heart rate slowly increase as the anesthesia wanes immediately after surgery.9)
Hypertensive patients are more likely to experience BP fluctuations during the operation, which may lead to myocardial ischemia.6) European guidelines recommend that perioperative BP be maintained at 70–100% of the baseline to prevent excessive tachycardia.6) The perioperative risk associated with HT varies depending on HT stage. However, most evidence regarding BP level and perioperative risk was from clinical studies prior to 1990, when there were few antihypertensive medications. It is also unclear whether postponing surgery to control BP in hypertensive patients can reduce this risk.
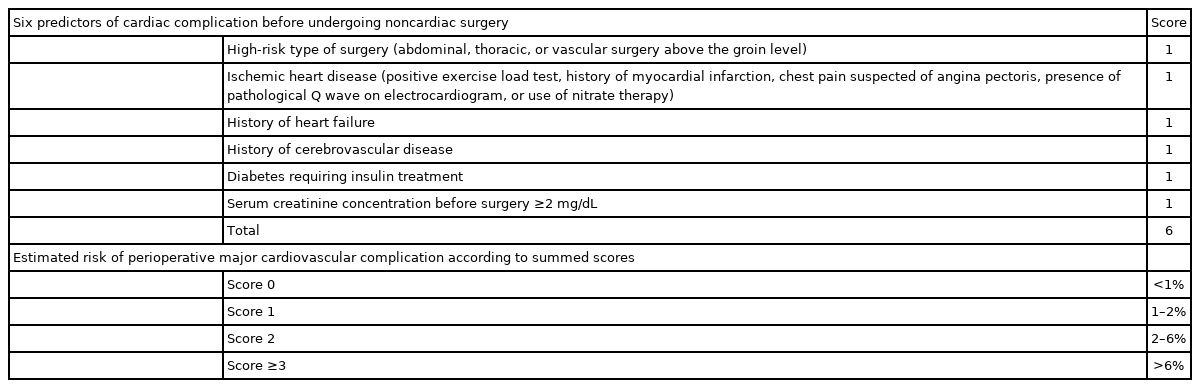
The most validated clinical risk index, known as the Revised Cardiac Risk Index (RCRI), includes 6 factors, each worth 1 score (Table 1).10) The results showed risk estimates of myocardial infarction, ventricular fibrillation or cardiac arrest, pulmonary edema, and complete heart block of 0.5% (95% confidence interval [CI], 0.2–1.1%) for an RCRI score of 0, 1.3% (95% CI, 0.7–2.1%) for an RCRI score of 1, 3.6% (95% CI, 2.1–5.6%) for an RCRI score of 2, and 9.1% (95% CI, 5.5–13.8%) for an RCRI score ≥3.10) The RCRI showed moderate discrimination in predicting major perioperative cardiac complications in a large sample systematic review.11) The RCRI stratified patients with low-risk (<1%) and higher risk (≥1%) for perioperative major adverse cardiovascular events during surgical hospital admission or within 30 days of surgery. Although HT itself is not considered as a main component of RCRI, HT requiring medication was counted as one of the 21 preoperative components to predict postoperative complications in the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP).12) Although the ACS NSQIP surgical risk calculator is more complex than RCRI, it may provide better predictive discrimination.13)
Perioperative risk is divided into two categories according to the stage of HT. One is severe HT, in which case it is recommended that the surgery be postponed.6) Severe HT is defined as high systolic/diastolic BP ≥180/110 mmHg, new identification of HT-mediated organ damage, or suspicion of secondary HT without proper diagnosis.6) Patients with severe HT who did not take antihypertensive medication showed an exaggerated BP change during induction and operative procedures.14)15) In other studies, preoperative diastolic BP >110 mmHg has been associated with various complications such as arrhythmia, myocardial ischemia, myocardial infarction, and heart failure; therefore, it is reasonable to recommend surgery after controlling BP.16)17)
In contrast, in patients with mild to moderate HT with systolic/diastolic BP <180/110 mmHg, there is no evidence of the benefit of postponing surgery to optimize therapy.6)7) HT with a diastolic BP of less than 110 mmHg does not appear to increase the risk of surgery.6) Therefore, it is safe to recommend that BP be carefully monitored during and after the operation without delaying the surgery.
PERIOPERATIVE MANAGEMENT OF HYPERTENSIVE PATIENTS TAKING ANTIHYPERTENSIVE MEDICATION
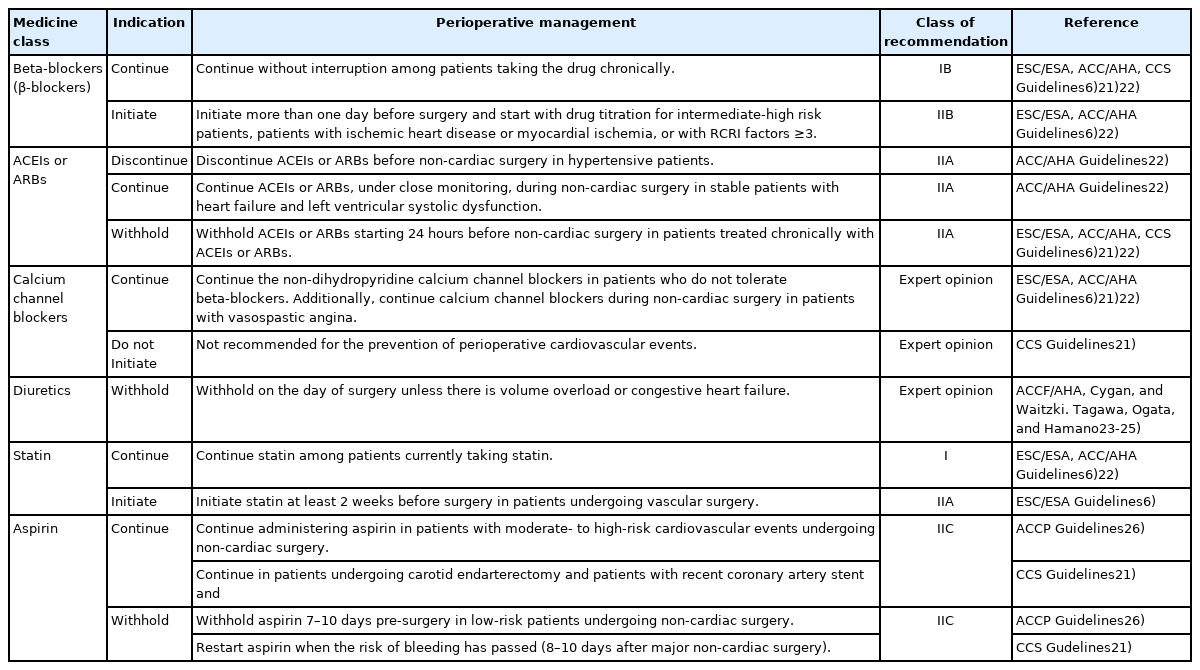
In principle, oral antihypertensive drugs should be continued until the point of surgery. Beta-blockers or clonidine, in particular, can cause severe repulsive BP rise if abruptly stopped before surgery.18-20) It is recommended that most antihypertensive medications be taken with a small amount of water, even on the morning of surgery. However, in the case of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs), it is recommended to stop them for 24 hours before surgery.21) The recent recommendation guidelines and evidence of antihypertensive medications are presented in Figure 1 and summarized in Table 2. The following is a summary of the recommendations for antihypertensive drugs in each group.

Perioperative antihypertensive medicine summary.
ACEIs = angiotensin-converting enzyme inhibitors; ARBs = angiotensin receptor blockers.
*Initiate more than one day before surgery and start with drug titration for intermediate-high-risk patients, patients with ischemic heart disease or myocardial ischemia, or with revised cardiac risk index factors ≥3; †Discontinue ACEIs or ARBs before non-cardiac surgery in hypertensive patients. However, in stable patients with heart failure and left ventricular systolic dysfunction, continuing these drugs should be considered; ‡Continue receiving aspirin in patients with moderate- to high-risk cardiovascular events undergoing non-cardiac surgery; §Withhold aspirin 7–10 days before surgery in low-risk patients undergoing noncardiac surgery. Aspirin is started when the risk of bleeding has passed (8–10 days after major non-cardiac surgery). Individualized maintenance in patients with previous cardiovascular interventions.
Beta-blockers
Beta-blockers are standard therapy for congestive heart failure, HT, ischemic heart disease, and arrhythmia disease.1)2)6)22) Beta-receptors in the human body consist of three subtypes: β1-, β2-, and β3-receptors. β1-receptors are predominant in cardiac tissue. Stimulation of these receptors increases cardiac output by causing positive chronotropic and inotropic effects.27) β2-receptors are found particularly in the smooth muscles of vascular and pulmonary tissue.27) They induce vasodilation and bronchodilation in the heart and cause myocytes to increase heart rate and contractility. β3-receptors are located in adipose tissue and skeletal muscle, and their activation causes lipolysis and thermogenesis.27) In the case of beta-blockers, bisoprolol and atenolol, which have high beta-1 selectivity, are preferentially recommended to prevent bronchoconstriction during surgery.28-30)
There is a consensus that hypertensive patients should continue beta-blocker medication when undergoing surgery.22) According to a nationwide cohort study by Andersson et al.,31) beta-blockers have the advantage of reducing the risk of major adverse cardiac events within 30 days of follow-up after surgery among patients with myocardial ischemia who underwent non-cardiac surgery. They equally reduce mortality among those with heart failure and recent myocardial infarction. Beta-blockers have been reported to reduce myocardial ischemia and myocardial infarction during non-cardiac surgery in multiple meta-analyses.32-35) Betablockers significantly reduce atrial fibrillation and ventricular arrhythmias within 30 days of follow-up after surgery and may have little or no effect on bradycardia and hypotension.36)37) Therefore, their intake should be continued during surgery. In particular, in patients with coronary artery disease, sudden discontinuation of beta-blockers before surgery can cause angina pectoris, myocardial infarction, or sudden death.
There is still controversy regarding whether adding new beta-blockers before surgery will be helpful. It has been reported in particular that adding high-dose beta-blockers immediately before surgery increases the risk of mortality, in part because of the higher incidence of stroke, hypotension, and bradycardia.38) Therefore, if beta-blockers are added to high-risk patients, it is recommended to start with a margin of at least 24 hours before surgery and adjust the dose with an adaptation period, preferably for a week or so.13) If repeated, starting new beta-blockers on the morning of the surgery should be avoided.
ACEIs/ARBs
It is recommended to withhold ACEIs and ARBs for 24 hours before surgery unless it is difficult to stop the medication due to heart failure or severe HT.6)21) This recommendation is because long-term hypotension can be induced if the compensatory action of the reninangiotensin system is inhibited during surgery.39)40) Indeed, this recommendation is in conjunction with recent prospective international cohort studies, the Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) study.41) The VISION study included 16,079 patients aged >45 years from 8 countries: Asian, Australian, European, North, and South American from 2007 to 2011.41) This cohort showed evidence that patients who took ACEIs/ARBs at baseline, then withheld their ACEIs/ARBs in the 24 hours prior to surgery had an 18% relative risk reduction of the composite outcome of death, stroke, and myocardial injury after non-cardiac surgery, compared to patients who continued the medication (relative risk, 0.82; 95% CI, 0.70–0.96; p=0.01).41) A recent meta-analysis pooled 13 published papers (3 randomized control trials and 10 observational studies) which showed that patients who continued consuming the ACEIs/ARBs were significantly prone to developing hypotension when under anesthesia, with a relative risk of 41%.42) Usually, it is recommended to take the ACEIs or ARBs until the morning of the day before surgery, to stop intake on the day of surgery, and resume intake the day after surgery if the vital signs are stable.21) On the other hand, it is recommended to continue intake for as long as possible in the case of heart failure patients, even during surgery, and restart as soon as possible, if intake was stopped.6)
Despite the recommendations mentioned earlier, the American College of Cardiology/ American Heart Association (ACC/AHA) guidelines indicate that it is reasonable to continue ACEI or ARB therapy; this differs from the recommendations of the European and Canadian Guidelines.22) This recommendation was based on a large observational retrospective study of 79,228 patients who underwent non-cardiac surgery and was analyzed with propensity score matching between patients on ACEIs and those not on ACEIs.43) In this matched cohort study, there was no association between ACEI administration and respiratory morbidity after surgery as the primary outcome and no association with 30-day mortality and composite in-hospital mortality and morbidity as a secondary outcome; however, intraoperative hypotension was more common in patients taking ACEIs.43) This study included patients with low-risk and highrisk surgeries, while other previous studies were limited to high-risk surgeries.43) This study suggests that it is reasonable to continue ACEI medication for minor risk surgeries.
Calcium channel blockers
In the case of calcium blockers, the incidence of postoperative bleeding may be increased by inhibiting platelet aggregation, and bleeding may worsen by interfering with compensatory vasoconstriction.44) Nevertheless, it is recommended to continue intake because the benefits of BP control outweigh the damage.6)
Diuretics
In a recent observational study by Tagawa et al.,23) evaluating 2,725 subjects who underwent noncardiac surgery, perioperative diuretic administration was associated with a risk of postoperative acute kidney injury by 2.07 (95% CI, 1.10–3.89; p=0.02). There is no consistent recommendation on whether diuretics should be withheld before surgery. However, it is usually recommended to withhold them on the day of surgery if the risk of BP elevation is low.45) It was reported that withholding diuretics on the day of surgery reduced the risk of acute kidney injury.23)
Statins and aspirin
Statins and aspirin are frequently prescribed medications for patients with hypertension. The perioperative use of statins is suggested to have a beneficial effect. A meta-analysis of 35 randomized control trials, including 8,200 patients, showed that statin therapy has a protective effect on postoperative myocardial infarction in non-cardiac surgery by 64% (odds ratio, 0.44; 95% CI, 0.3–0.64).46) Therefore, statins should be continued in those on treatment. Moreover, statins should be initiated at least 2 weeks before surgery in patients undergoing vascular surgery or in patients with clinical risk factors undergoing an elevated-risk procedure.47-49)
Aspirin use in the perioperative period remains a contentious debate. The Perioperative Ischemic Evaluation 2 trial was a multinational, randomized controlled trial (RCT) that observed the outcome of 10,010 patients undergoing non-cardiac surgery on low-dose aspirin vs. placebo.50) The patients were stratified according to the 5,628 patients with aspirin initiation and 4,382 patients with aspirin continuation.50) Aspirin did not reduce mortality or non-fatal myocardial infarction rates at 30 days follow-up after non-cardiac surgery.50) However, major bleeding was more common in the aspirin group than in the placebo group. The primary and secondary results were comparable in either the initiation or continuation aspirin group.50) Therefore, it is not recommended to initiate or continue aspirin use during non-cardiac surgery. In contrast, in a RCT with 220 subjects, with at least one cardiac risk factor, undergoing high-to-intermediate risk non-cardiac surgery, treatment with low-dose aspirin seven days before surgery and three days post-surgery, compared to placebo, reduced the absolute and relative risks of post-surgery major adverse cardiovascular events by 7.2% and 80% respectively. Notably, there was no increase in perioperative bleeding between the aspirin and placebo groups (median perioperative estimated blood loss: 300 mL vs. 300 mL, p=0.61).51)
The American College of Chest Physicians (ACCP) guidelines recommend withholding aspirin 7–10 days prior to low-risk, non-cardiac surgery.26) In contrast, moderate to high-risk patients undergoing non-cardiac surgery are recommended to continue aspirin around the time of surgery.26) The Canadian Cardiovascular Society Guidelines recommend withholding aspirin at least 3 days prior to surgery, except for patients who undergo carotid endarterectomy and for patients after recent coronary stent implantation. It is equally recommended to restart aspirin intake when the period for bleeding risk related to surgery has passed.21)
CONCLUSION
Severe HT ≥180/110 mmHg can increase the risk of surgery. Therefore, sufficient BP control prior to the surgery is recommended. In general, oral hypertensive medication should be continued before and after surgery. In particular, sympathetic blockers, such as beta-blockers, must be continued. However, it is recommended to stop taking ACEI and ARB 24 hours before surgery because they can inhibit excessive compensatory renin-angiotensin activation during surgery. It is strongly recommended to continue with statins during surgery, whereas it is recommended to withhold aspirin in order to minimize the risk of bleeding.
Notes
Conflict of Interest
The authors have no financial conflicts of interest.
Author Contributions
Conceptualization: Rismiati H, Lee HY; Supervision: Lee HY; Writing - original draft: Rismiati H; Writing - review & editing: Rismiati H, Lee HY.