ABSTRACT
- Previous researchers have suggested that people with disabilities have a higher prevalence and risk of type 2 diabetes mellitus than the general population. As diabetes is a well-known risk factor for cardiovascular disease (CVD), developing strategies to prevent and delay its occurrence in people with disabilities is important to reduce the burden of CVD. However, people with disabilities are often excluded from studies and have received little attention from public health authorities and researchers. These unmet needs for health care and being left out of research may affect the progression of diabetes in people with disabilities. Herein, we would like to briefly discuss the increased risk of diabetes and related conditions in people with disabilities and suggest that more attention should be given to this population.
-
Keywords: Cardiovascular disease; Diabetes mellitus; Disabled persons
INTRODUCTION
- With the improvement of medical technology, most developed countries have entered an aging society, and the population with disabilities is constantly increasing. Disability is defined by the International Classification of Functioning, Disability, and Health as the state of having limitations in body functions, structures, activities, and participation.1) People with disabilities comprise up to 26% of adults in the United States2) and 5.6% of the Korean population in 2014.3) In relation, medical expenditures have also been increasing. The national disability-associated health care expenditures have increased by approximately 65% over the past decade in the United States.4) With the improved life expectancy in the future, the prevalence of chronic diseases such as type 2 diabetes mellitus (T2DM) in the disabled is also expected to increase.5) Given that diabetes is a well-known risk factor for cardiovascular disease (CVD), the risk of CVD is expected to increase in people with disabilities. Previous studies have suggested that people with disabilities have higher CVD risk and mortality compared to the general population.6) As the burden on individuals and society increases due to chronic medical conditions associated with CVD, developing strategies for preventing the occurrence of T2DM in people with disabilities is important to reduce the burden of CVD.
EPIDEMIOLOGY OF DIABETES IN PATIENTS WITH DISABILITIES
- Existing studies have reported that people with disabilities have a higher prevalence of diabetes and risk of diabetes than the general population.5) Most study designs were unable to distinguish between type 1 diabetes mellitus and T2DM. However, the overall proportion of T2DM was approximately 90% of all the patients with diabetes.7) According to Jung et al.,8) people with disabilities in South Korea had a 34% increased risk of having diabetes (odds ratio [OR], 1.34; 95% confidence interval, 1.33–1.34; p<0.001), and a higher OR of T2DM was observed in people with severe disabilities compared to people with mild disabilities. In a Swedish national registry-based study, people with intellectual disabilities were 20% more likely to have a diagnosis of diabetes than the general population.9) Among those with diabetes, intellectual disability was associated with a higher rate of insulin prescription.9) MacRae et al.10) conducted a systematic review and suggested an overall increase in the prevalence of diabetes in people with intellectual disabilities.
DISABILITIES AND OBESITY
- Epidemiologic studies have also shown that the prevalence of obesity may be higher in people with disabilities than in the general population.10-12) Kinne et al.13) reported that the prevalence of weight or eating problems was higher in the group with disabilities than in the general population (adjusted OR, 2.96). The mechanisms by which obesity occurs in people with disabilities are not clear, but pathophysiological changes with decreased energy expenditure that result in a positive energy balance may play a key role.12) Changes in the body composition of people with physical disabilities are associated with reduced energy expenditure. Several studies have reported decreased fat-free mass and increased fat mass in people with disabilities.14)15) As such, these changes in the body composition in obese individuals may result in insulin resistance and T2DM.
DISABILITIES AND CVD
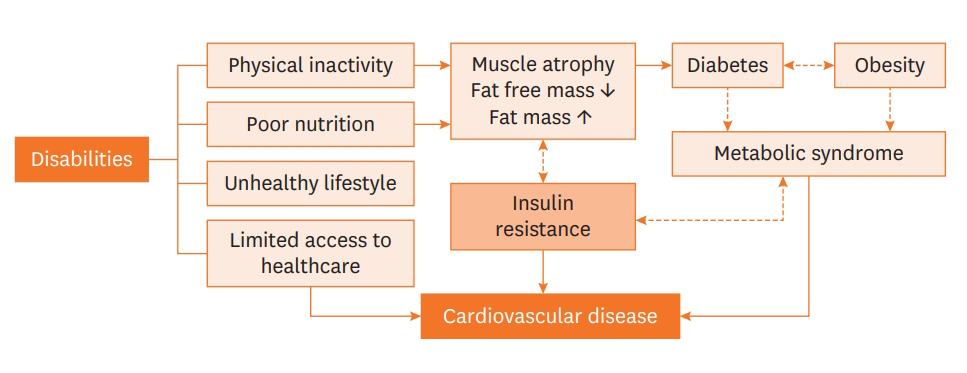
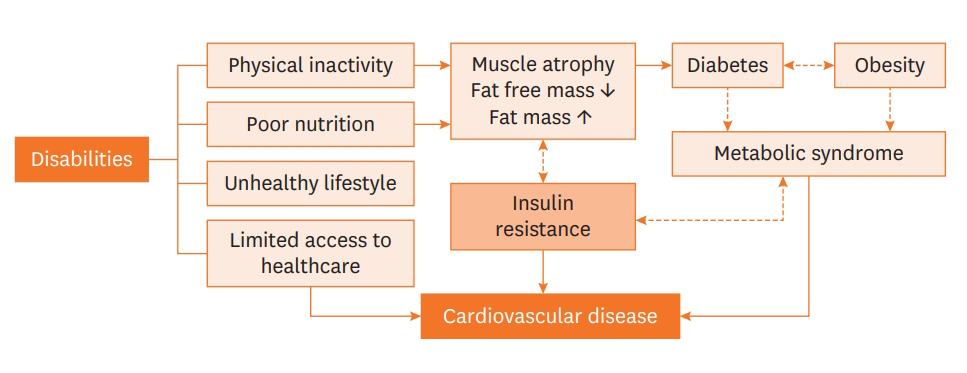
- Despite the increasing trends of diabetes and the associated medical conditions among people with disabilities, people with disabilities are often excluded from epidemiological research and have received little attention. To our knowledge, the incidence and mortality of CVD increase in people with disabilities, regardless of the type or severity of their disability.6) Interestingly, the increase in cardiovascular mortality was more evident in young people with disabilities. Diabetes and obesity are strongly associated with an increased risk of CVD, such as myocardial infarction or stroke. In addition, compared with the general population, people with disabilities are more likely to have unhealthy diets16) and a sedentary lifestyle with limited physical activity.17)18) A diagram describing the hypothetical mechanism of CVD development in people with disabilities is shown in Figure 1.
BARRIERS AND CHALLENGES
- As mentioned above, the prevalence and risk of diabetes and CVD are significantly higher in people with disabilities than in those without. However, there are disparities and unmet needs for people with disabilities in terms of access to health care, which may affect the progression of diabetes. According to previous studies on medical accessibility and disparities among people with disabilities, it is often difficult for them to visit healthcare professionals due to their limited income and restrictions in mobility.19)20) In addition, exercise or nutritional education programs for the prevention of diabetes have been developed for people without disabilities. Similarly, online or visiting education programs for people with disabilities should also be developed. Physical disabilities make it impossible to participate in exercise programs designed for the general population. Therefore, it is important to educate guardians and develop exercise rehabilitation programs suitable for the special situation of individuals with disabilities.
CONCLUSIONS
- As life expectancy increases, it is necessary to identify diabetes and associated health factors among people with disabilities, which are associated with the risk of CVD. Physicians and policymakers should pay more attention to people with disabilities to ensure the prevention and proper management of diabetes in this population.
ARTICLE INFORMATION
-
Conflict of Interest
The authors have no financial conflicts of interest.
-
Author Contributions
Writing - original draft: Jung I, Rhee EJ, Lee WY.
Figure 1.Possible mechanism of the development of cardiovascular disease in people with disabilities.
REFERENCES
- 1. World Health Organization. International Classification of Functioning, Disability and Health: Children & Youth Version: ICF-CY. Geneva, World Health Organization; 2007.
- 2. Sabatello M, Landes SD, McDonald KE. People with disabilities in COVID-19: Fixing our priorities. Am J Bioeth 2020;20:187–90.ArticlePubMedPMC
- 3. Lee JE, Kim HR, Shin HI. Accessibility of medical services for persons with disabilities: comparison with the general population in Korea. Disabil Rehabil 2014;36:1728–34.ArticlePubMed
- 4. Khavjou OA, Anderson WL, Honeycutt AA, Bates LG, Razzaghi H, Hollis ND, Grosse SD. National health care expenditures associated with disability. Med Care 2020;58:826–32.ArticlePubMedPMC
- 5. Cooper SA, Hughes-McCormack L, Greenlaw N, McConnachie A, Allan L, Baltzer M, McArthur L, Henderson A, Melville C, McSkimming P, Morrison J. Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: a population-based cohort study. J Appl Res Intellect Disabil 2018;31 Suppl 1:68–81.ArticlePubMed
- 6. Son KY, Kim SH, Sunwoo S, Lee JY, Lim S, Kim YS. Association between disability and cardiovascular event and mortality: a nationwide representative longitudinal study in Korea. PLoS One 2020;15:e0236665.ArticlePubMedPMC
- 7. National Institute for Health and Care Excellence (NICE). Type 2 Diabetes. Full Guidance, 26 January 2011. London, NICE; 2013.
- 8. Jung I, Kwon H, Park SE, Han KD, Park YG, Rhee EJ, Lee WY. The prevalence and risk of type 2 diabetes in adults with disabilities in Korea. Endocrinol Metab (Seoul) 2020;35:552–61.ArticlePubMedPMC
- 9. Axmon A, Ahlström G, Höglund P. Prevalence and treatment of diabetes mellitus and hypertension among older adults with intellectual disability in comparison with the general population. BMC Geriatr 2017;17:272. ArticlePubMedPMC
- 10. MacRae S, Brown M, Karatzias T, Taggart L, Truesdale-Kennedy M, Walley R, Sierka A, Northway R, Carey M, Davies M. Diabetes in people with intellectual disabilities: a systematic review of the literature. Res Dev Disabil 2015;47:352–74.ArticlePubMed
- 11. Anderson WL, Wiener JM, Khatutsky G, Armour BS. Obesity and people with disabilities: the implications for health care expenditures. Obesity (Silver Spring) 2013;21:E798–804.ArticlePubMedPMC
- 12. Liou TH, Pi-Sunyer FX, Laferrère B. Physical disability and obesity. Nutr Rev 2005;63:321–31.ArticlePubMed
- 13. Kinne S, Patrick DL, Doyle DL. Prevalence of secondary conditions among people with disabilities. Am J Public Health 2004;94:443–5.ArticlePubMedPMC
- 14. Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testolin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol 2003;40 Suppl 1:S183–6.ArticlePubMed
- 15. Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil 2003;84:1068–71.PubMed
- 16. Hoey E, Staines A, Walsh D, Corby D, Bowers K, Belton S, Meegan S, McVeigh T, McKeon M, Trépel D, Griffin P, Sweeney MR. An examination of the nutritional intake and anthropometric status of individuals with intellectual disabilities: results from the SOPHIE study. J Intellect Disabil 2017;21:346–65.ArticlePubMed
- 17. Bartlo P, Klein PJ. Physical activity benefits and needs in adults with intellectual disabilities: systematic review of the literature. Am J Intellect Dev Disabil 2011;116:220–32.ArticlePubMed
- 18. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003;289:76–9.ArticlePubMed
- 19. Hwang B, Chun SM, Park JH, Shin HI. Unmet healthcare needs in people with disabilities: comparison with the general population in Korea. Ann Rehabil Med 2011;35:627–35.ArticlePubMedPMC
- 20. McColl MA, Jarzynowska A, Shortt S. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc 2010;25:205–18.Article
Citations
Citations to this article as recorded by

 , Eun-Jung Rhee, MD, PhD
, Eun-Jung Rhee, MD, PhD , Won-Young Lee, MD, PhD
, Won-Young Lee, MD, PhD