ABSTRACT
- Catheter ablation for atrial fibrillation (AF), especially pulmonary vein (PV) isolation, is widely used for rhythm control. However, AF recurrence remains a challenge, affecting 20% to 50% of cases. This review focuses on AF recurrence after catheter ablation. AF recurrence can be categorized into early recurrence (ER) within 3 months after index procedure, late recurrence (LR) within 1 year, and very LR (VLR) occurring beyond 1 year. ER has emerged as a significant predictor of LR, contrary to the traditional understanding. LR is primarily caused by PV reconnection, while VLR more involves non-PV triggers or substrates. Managing AF recurrence includes antiarrhythmic drugs, steroids, colchicine, and repeat ablation. Antiarrhythmic drugs reduce ER but have a limited impact on LR. Steroids have been shown to reduce ER, but not long-term recurrence. Colchicine, an anti-inflammatory agent, shows promise in reducing both ER and LR, although further research is necessary. Whether to perform early repeat ablation after ER remains uncertain, as not all patients require immediate intervention. In conclusion, AF recurrence after ablation remains a complex issue. Understanding the underlying mechanisms is essential for personalized management. Tailored approaches, considering individual characteristics, are crucial for long-term success. Future research should focus on improving therapeutic strategies for AF recurrence.
-
Keywords: Atrial fibrillation; Catheter ablation; Recurrence
INTRODUCTION
- Atrial fibrillation (AF) is the most common arrhythmia; it requires sustained treatment and is a leading cause of a variety of morbidities. The mainstream of AF management is the “ABC pathway,” as outlined in a recent guideline [1,2]. In particular, the importance of rhythm control for improved symptoms has been increasingly emphasized. The EAST-AFNET 4 (Early Therapy of Atrial Fibrillation for Stroke Prevention Trial) Study [3] demonstrated that early rhythm control significantly improved composite cardiovascular outcomes compared to the usual care group. Those results have justified active attempts for rhythm control. Currently, catheter ablation for effective rhythm control is widely utilized. Stemming from the pioneering work of Haissaguerre et al. [4], pulmonary vein (PV) isolation by radiofrequency (RF) catheter ablation has become a cornerstone of AF ablation. Furthermore, other than RF energy, cryoablation and pulsed field ablation are also effectively employed for PV isolation. Numerous previous studies have confirmed that catheter ablation for rhythm control is more effective than medical rhythm control [5–7]. However, a persistent issue is the recurrence of AF. AF recurrences after catheter ablation are common, with estimates ranging from 20% to 50% after 5 years [8]. There is limited guidance available for decision-making or for managing AF recurrence after catheter ablation. Therefore, we present a review of the etiology of AF recurrence after catheter ablation, the characteristics of atrial electrical remodeling in the redo procedure, and management options for AF recurrence.
DEFINITION OF AF RECURRENCE
- Early recurrence
- Early recurrence (ER) refers to the recurrence of AF within 3 months after ablation, and it is known to occur in approximately 50% of patients postprocedure. In an expert consensus on catheter and surgical ablation of AF, ER is defined as recurrence of atrial tachyarrhythmia—comprising AF, atrial flutter (AFL), and atrial tachycardia (AT)—within 3 months after ablation [8]. This period is often referred to as the blanking period, a term that has been defined differently across various studies, with durations ranging from 1 week to 3 months [9–13]. This diversity in blanking periods has made it challenging to standardize the definition. In the expert consensus statements, the task force team agreed to define the blanking period as the first 3 months postprocedure, during which any recurrence of AF should not be considered a treatment failure. If a blanking period of less than 3 months is chosen, it should be prespecified and clearly stated. Previous studies have often attributed ER occurring shortly after the procedure to acute inflammatory reactions caused by RF energy application, transient imbalances in the autonomic nervous system, or the need for lesions created by RF energy to stabilize over time [14–16]. All of these factors were once thought to be reversible.
- Recent studies have consistently provided evidence that ER can be a significant predictor of late recurrence (LR) beyond 1 year, challenging the traditional understanding of ER. Kim et al. [17] conducted a retrospective analysis and found that 24.1% of patients experienced ER. In a multivariate analysis, ER was identified as an independent predictive factor for LR following a single procedure, with a hazard ratio (HR) of 2.76. This trend was consistent regardless of whether the AF type was paroxysmal or nonparoxysmal. Several substudies of large randomized trials have also reported similar findings. In a substudy of the ADVICE (Adenosine Following Pulmonary Vein Isolation to Target Dormant Conduction Elimination) Trial [18], 49.1% of patients who underwent RF catheter ablation experienced ER of atrial tachyarrhythmia, including AF/AT, and among these patients, those who experienced ER had a significantly higher incidence of LR (HR, 4.80). Andrade et al. [19] analyzed a subgroup of the STAR-AF (Substrate and Trigger Ablation for Reduction of Atrial Fibrillation) Trial and found that 49% of patients experienced ER. During a 1-year follow-up period, the group of patients who experienced ER had a significantly higher incidence of LR (66.7%) than the group that did not experience ER (28.6%). Not only RF catheter ablation, but also cryoablation has shown a considerable rate of ER, which was a strong predictor for LR. Park et al. [20] analyzed 406 patients who underwent cryoablation at two tertiary institutions. Of these patients, 161 (39.7%) had paroxysmal AF, and 104 (25.6%) experienced ER. The group of patients with ER had a significantly higher incidence of LR at 1 year.
- The timing of ER appears to influence the incidence of LR in distinct ways. In a study of paroxysmal AF [21], it was noted that patients who experienced their first recurrence within the first 3 months had a lower incidence of LR. Similarly, other studies have shown that patients who had a recurrence within the first month exhibited fewer instances of LR than those who experienced recurrence in the second or third month [18,22]. Conversely, in a study of persistent AF, this temporal difference seemed to have less of an impact. The authors of that study speculated that this might be due to variations in the underlying mechanisms of recurrence. They suggested that paroxysmal AF might be more influenced by transient factors, while persistent AF might be more closely associated with substrate-related factors, leading to recurrence [23].
- Late recurrence
- LR is defined as recurrence within 1 year, excluding the first 3 months following the index procedure (referred to as the blanking period) [8]. Recurrence after ablation usually occurs within 1 year, especially within 6 months, and the annual recurrence rate ranges from 5% to 9% [24,25]. LR has been reported to occur in 25% to 40% of cases, and this rate seems to vary among studies because of differences in patient population (paroxysmal vs. persistent, monitoring methods, follow-up duration, and study designs) [26,27]. PV reconnection is a main mechanism in many cases [26]. Numerous studies have reported factors predicting LR, with advanced age, male sex, left atrium size, and ER being commonly recognized as influential factors [28–33].
- Very late recurrence
- Very LR (VLR), defined as recurrence occurring 1 year or more after the index procedure, has an annual rate of 7.6% [8]. It has been noted that the recurrence rate tends to increase as the follow-up period extends [24,34]. While PV reconnection remains the primary cause, accounting for approximately 50% to 70% of cases, this cause is less common than it is for LR [24,35–37]. Sotomi et al. [35] compared the electrophysiologic characteristics in redo procedures for recurrent AF between LR and VLR. In that study, 124 with LR and 26 with VLR, PV reconnection was significantly lower in the VLR group (90% vs. 69%, P<0.01). Moreover, among the reconnected PV, the trigger that initiated the atrial tachyarrhythmia was significantly lower in the VLR group. The authors suggested that not only PV reconnection, but also the progression of the AF substrate, might be an important mechanism explaining VLR. Similar findings were also observed in Korean data. Choi et al. [38] reported that during a follow-up period of more than 5 years, the extra-PV trigger significantly increased in a patient group who experienced AF recurrence after 5 years from the initial procedure.
- One intriguing study [39] suggests that in instances where sinus rhythm is sustained for an extended period, there tends to be a more favorable response to direct current (DC) cardioversion or antiarrhythmic drugs, even without the necessity for repeat ablation. It is worth noting that repeat ablation has also demonstrated improved response rates in these patients. In another study [40], a considerable proportion of patients with PV reconnection have been observed to remain AF-free, suggesting that factors beyond PV triggers may influence AF occurrence in patients with long-term maintenance of sinus rhythm.
- Baseline characteristics for recurrence
- Previous studies have analyzed various risk factors for the recurrence of AF. Although there may be minor differences across studies, the most notable risk factors include the size of the left atrium (LA), the duration of AF, age, and epicardial fat [1]. In one meta-analysis [41], LA size >50 mm was a strong predictor of LR (odds ratio, 5.10; 95% CI, 2.00–12.9), and another research [42] also emphasized the significance of LA size and hypertension as important factors associated with recurrence. LA size and volume, especially when measured using computed tomography, were found to be associated with recurrence in studies with over 2 years of follow-up (VLR) [43–45]. Additionally, epicardial fat was found to impact both LR and VLR [46]. Other factors, such as prolonged P wave duration, high body mass index, extended interatrial conduction time, and social factors like low educational attainment, low family income, and living alone, were also associated with AF recurrence following ablation [47–49].
- Type of recurrence: AF, AFL, and AT
- The definition of recurrence varies across studies. Some studies consider only AF as recurrence, while others include all forms of atrial tachyarrhythmia, such as AFL or AT. For instance, the current expert consensus statement defines atrial tachyarrhythmia, including AF, AT and AFL, as recurrence. The reported frequency of recurrence ranges from 4.7% to 31%, reflecting the impact of different ablation methods and extents during the index procedure [50–52].
- The mechanism of AFL and AT recurrence is primarily related to PV reconnection or conduction delay/conduction block occurring in previously ablated lesions, leading to reentry. In prior studies, it appeared to be more favorable clinical course if the recurrence was as AFL and AT. One study involving 341 ablation cases [53], AFL and AT recurrence was reported in 10 individuals (3%), mostly associated with PV reconnection, and curative outcomes were achieved during redo procedures. Choi et al. [52] analyzed 133 redo procedure patients and found that 50 (37.6%) experienced AT recurrence and 83 (62.4%) experienced AF recurrence. The frequency of PV reconnection did not show significant differences between the two groups, while atrial arrhythmia-free survival was significantly better in the AT recurrence group. The main mechanisms of AT were predominantly related to perimitral flutter, followed by roof flutter and cavotricuspid isthmus flutter, with the exception of PV-related flutter. In addition, there were cases of focal AT from the vein of Marshal, septum, coronary sinus, and superior vena cava (SVC).
- In most cases of AFL and AT recurrence, the initial treatment typically involves DC cardioversion or antiarrhythmic drugs, which have often demonstrated favorable outcomes. However, these tachyarrhythmias may lead to worsening symptoms due to an increased mean ventricular rate (often a 2:1 ventricular response) compared to AF. Therefore, if the arrhythmia persists or frequently recurs, it may be reasonable to consider repeated ablation as a treatment option.
MEDICAL MANAGEMENT FOR AF RECURRENCE
- Antiarrhythmic drugs
- The association between ER and LR has led some researchers to investigate the potential effectiveness of reducing ER through antiarrhythmic drug therapy. Among these studies, the 5A Study [54] focused on 110 patients with paroxysmal AF who had undergone postprocedural antiarrhythmic drug therapy for 6 weeks. This resulted in a significant reduction in ER (13% vs. 28%), but no significant difference in LR was observed (72% vs. 68%). Similar trends were noted in the AMIO-CAT (Short-term Amiodarone Treatment after Catheter Ablation for Atrial Fibrillation) Trial [55] and the EAST-AF (Efficacy of Antiarrhythmic Drugs Short-Term Use After Catheter Ablation for Atrial Fibrillation) Trial [56], suggesting that while postablation antiarrhythmic drugs may have some effect in decreasing ER, their impact on recurrence beyond 3 months seems minimal. Even the meta-analysis data [57] did not show any statistically significant benefits. Therefore, the prescription of postprocedural antiarrhythmic drugs should be approached with caution, taking into account both the potential benefits and side effects, rather than being prescribed routinely.
- Steroids
- Given that acute inflammatory reactions are a key mechanism contributing to ER, it has been hypothesized that administering anti-inflammatory steroids immediately postprocedure could reduce such recurrences. Numerous studies have been undertaken to test this theory. According to research by Kim et al. [58], steroids were found to be significant in reducing ER, but they did not significantly impact recurrences at the 24-month mark. Recent data [59] has indicated that while steroids can decrease the inflammatory marker, they do not improve recurrence rates, regardless of whether the recurrence is early or late. Therefore, the routine prescription of steroids following an ablation procedure is not currently recommended.
- Colchicine
- The concept that AF recurrence is due to inflammatory reactions has led to the investigation of the anti-inflammatory agent colchicine. Two studies [60,61] have yielded promising results, demonstrating a reduction in ER and potential for reducing LR as well. Colchicine also decreased inflammatory markers. According to Deftereos et al. [61], early AF recurrence is mediated by an inflammatory process, and colchicine exerts its anti-inflammatory effect by inhibiting microtubule depolymerization. This inhibition simultaneously negatively impacts the phosphorylation of calcium channels, ultimately reducing calcium overload-induced tachyarrhythmia. Thus, colchicine appears to have a protective effect against AF recurrence. In an animal study [62], colchicine was associated with reduced myocardial fibrosis, which could potentially influence long-term AF recurrence. However, due to the relatively small sample size, varying dosing strategies, and diverse study endpoints, the current expert consensus has not issued a definitive recommendation regarding colchicine. A recent meta-analysis [63] indicated that colchicine not only tends to inhibit ER, but may also inhibit LR, as suggested by some previous studies. However, a significant number of patients taking colchicine were unable to maintain adherence to the prescribed duration as planned in the study, and discontinued use due to adverse effects of the drug. Given the adverse effects of colchicine, careful consideration is necessary before its administration. Moreover, due to the absence of large-scale studies, further research is needed to establish its efficacy and safety.
- DC cardioversion
- DC cardioversion is frequently used to restore patients' rhythm to normal sinus rhythm following a recurrence after ablation. O'Donnell et al. [64] reported that clinical recovery post-PV isolation typically takes around 3 months, and there has been a documented delay effect of RF energy following ablation [16]. Animal studies have shown that during persistent AF, the atrial effective refractory period decreases, heart rate accelerates, and AF induction rates increase [65]. Therefore, it has been observed that electrical and structural changes continue during sustained AF, adversely affecting the atrial myocardium at both cellular and inflammatory levels [66]. In this scenario, a vicious cycle ensues, leading to further persistence of AF and contributing to significant fibrosis and chamber enlargement in the LA. Specifically, during the acute inflammatory phase postablation, the environment is thought to be particularly conducive to AF induction. There is a viewpoint that maintaining sinus rhythm until atrial lesion healing occurs could be beneficial for long-term outcomes [67]. However, the optimal timing for DC cardioversion remains unclear. Some studies suggest that early DC cardioversion during the ER phase is associated with better long-term outcomes [66,67]. In contrast, other research findings suggest that the impact of early cardioversion on LR may not be significantly correlated [68,69]. Current expert opinions performing DC cardioversion within 30 days if recurrence occurs postablation [8].
REDO PROCEDURE
- Early period
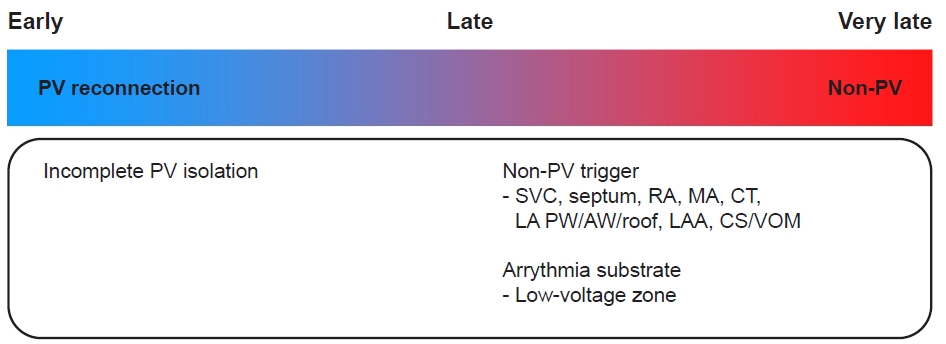
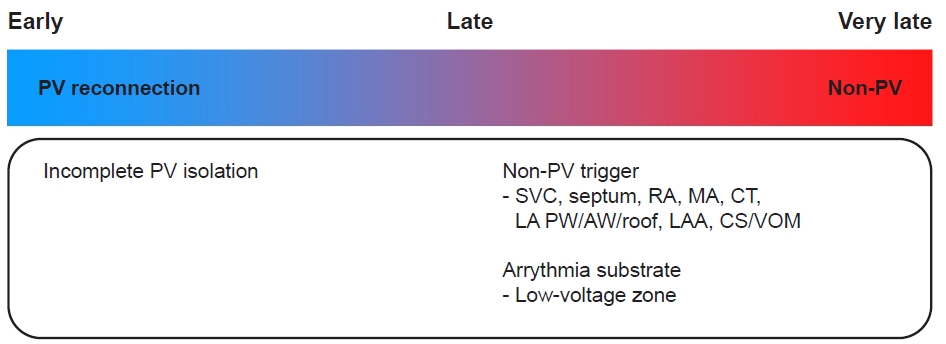
- The primary mechanism of ER is PV reconnection, as illustrated in Fig. 1. Electrophysiological testing conducted during early repeat ablation revealed that 88.2% of patients with ER exhibited PV reconnection. In contrast, PV reconnection was observed in only 41.7% of patients without ER [70].
- Whether to perform early repeat ablation in cases of ER remains unclear. In a study involving 302 patients [71], 158 experienced ER, with 151 of these included in the analysis. Of these, 61 patients underwent early repeat ablation within a month following the initial procedure, while the remaining 90 patients received standard care. All patients were given antiarrhythmic therapy for a month. If ER was present, the antiarrhythmic therapy was extended beyond a month. If symptoms persisted at the 3-month mark, antiarrhythmic therapy was continued until further ablation was performed. The group that underwent early repeat ablation demonstrated significantly lower recurrence rates during follow-up, but this was also linked to a significant increase in the total number of procedures. In a substudy of the STOP-AF (Sustained Treatment of Paroxysmal Atrial Fibrillation) Trial [72], out of 163 patients, 84 experienced ER, with 30 of them (36%) undergoing early repeat ablation during the blanking period. The use of antiarrhythmic drugs post–blanking period was discouraged. When compared to patient groups without ER, the AF-free survival rate was significantly higher in the early ablation group. The group with ER but without repeat ablation demonstrated the least favorable outcome. However, the authors noted that 55.6% of patients who experienced ER later had LR, while the remaining 44.4% did not experience LR despite having ER in this study. Therefore, they emphasized that not all patients with ER necessarily require immediate ablation. Instead, they suggested that considering the cost, the patient’s disease burden, and the risks associated with ablation, it might be more prudent to follow the expert consensus recommendation of waiting for 3 months before considering repeat ablation. Similar trends were observed in another study [21], where 51% had early atrial tachyarrhythmia and developed LR later, while the remaining 49% did not experience LR, a finding the authors considered noteworthy.
- If a recurrence happens during the blanking period, the decision to proceed with an immediate repeat ablation should be thoughtfully considered. This decision should take into account the ongoing presence of atrial arrhythmia, the patient's perceived disease burden, and potential mechanisms as indicated by the records from the initial procedure.
- Late period
- PV reconnection is also widely recognized as a primary mechanism of LR. A study involving 149 patients undergoing repeat procedures [73] found that electrophysiological testing during the first repeat ablation revealed PV reconnection in all patients. However, in subsequent procedures (second or third), the incidence of PV reconnection decreased, with a particularly notable reduction observed in persistent AF cases. Another study [74] reported PV reconnection in 73.2% of cases during repeat ablation. The importance PV reconnection as a contributing factor to recurrence appears to diminish as the timing of recurrence becomes more delayed (Fig. 1). Nevertheless, since PV reconnection plays a substantial role in a significant number of recurrence cases, it is crucial to assess the status of PV during repeat ablation.
- Very late period
- While PV reconnection is a widely recognized primary mechanism, non-PV triggers or substrates appear to be increasingly significant in the very late period (Fig. 1). Consequently, key predictive factors for VLR include nonparoxysmal forms of AF or underlying structural heart diseases (such as valvular or myocardial diseases), and advanced age at the time of the first ablation.
- In a study [36] that analyzed 137 patients who experienced recurrences after 36 months, electrophysiological testing during repeat ablation revealed PV reconnection in 81% of cases. However, a significant percentage of non-PV triggers were also discovered, including 35% from SVC, 45.9% from the posterior wall, and 51.82% from the roof. Other research [35] has also shown a trend towards a numerical decrease in PV triggers in the VLR group compared to non-VLR cases, although this was not statistically significant (77% vs. 82%). A recent study by Choi et al. [38], which had a 5-year follow-up, found that in patients who maintained sinus rhythm for more than 5 years, extra-PV triggers were more prevalent than PV reconnection. This suggests that while PV triggers may be crucial in the early stages of AF, as atrial cardiomyopathy progresses over time, the importance of extra-PV triggers increases.
- While PV reconnection is a significant factor, with potential causes such as gaps or a lack of transmural ablation lines during the index procedure, the coexistence of many PV reconnection cases with long-term sinus rhythm maintenance suggests that our understanding of the mechanisms underlying AF initiation and long-term maintenance is still uncertain. Therefore, it seems that the substrate plays a crucial role in VLR. In the study of Kim et al. [75], voltage mapping was performed during the index procedure. Based on these results, the authors divided the patients into four groups according to the extent of the low-voltage zone. They demonstrated that a higher prevalence of low-voltage zones was associated with a higher recurrence rate of AF at 3 years.
- Redo procedure vs. antiarrhythmic drugs
- A comparative study [76] was conducted to investigate the management of recurrent AF following the initial procedure, with a particular focus on the comparison between repeat ablation and antiarrhythmic drug therapy. The study scrutinized a cohort of 1,230 patients who underwent repeat procedures from a total of 4,913 patients who experienced AF recurrence in China. The primary endpoint, which included cardiovascular mortality, stroke, and major bleeding, showed significant improvement in the group that underwent repeat procedures. This result aligns with data from Swedish health registries [77]. However, it contrasts with previous findings from the ORBIT-AF (Outcomes Registry for Better Informed Treatment of Atrial Fibrillation) Trial [78], which did not demonstrate similar improvements in hard endpoints.
- Temporal trends
- An analysis of healthcare data from the United States [79] examined the decision-making process and timing of repeat ablation. Roughly 14.6% of patients with recurrent conditions underwent repeat ablation, with 12.1% of these patients receiving a second ablation within 1 year of the recurrence. Of this group, 20.6% underwent repeat ablation during the blanking period. Interestingly, social factors such as income level and residence in the southern United States had a more substantial influence on the decision to undergo repeat ablation than any particular clinical characteristics.
- A survey [80] was conducted to examine the current treatment trends for ER among contemporary physicians, specifically targeting 436 members of the European Heart Rhythm Association (EHRA). The survey sought information on the strategies used to manage ER. Of those who responded, 58% indicated that they did not adhere to the expert consensus guidelines for ER, choosing not to perform repeat ablation. When faced with the first AF recurrence during the blanking period, 62% of physicians opted for a combination of antiarrhythmic drugs and DC cardioversion, 17% employed rate control strategies, 20% performed only DC cardioversion, and a mere 1% selected repeat ablation. In instances of AFL/AT recurrence, there was a marked preference for repeat ablation, particularly when typical flutter was detected, with 51% of physicians choosing this treatment approach.
- In another survey study [81], 107 EHRA members were queried about their management strategies following a recurrence. The responses varied based on whether the recurrence was paroxysmal or persistent. PV isolation-only redo procedures were notably more prevalent in paroxysmal cases, while substrate modification was more frequently attempted in nonparoxysmal cases. There was also a difference in the rate control treatment approach, with 7% for paroxysmal cases and 21% for nonparoxysmal cases. The management strategies also exhibited slight variations. In paroxysmal AF cases, PV isolation was deemed the most critical, while for persistent AF, additional procedures such as low-voltage area ablation, complex fractionated atrial electrograms, empirical lines, and non-PV trigger ablation were also performed during redo procedures. Interestingly, a significant proportion of physicians adopted a conservative approach, either modifying or adding antiarrhythmic drugs. This indicates that a considerable number of clinicians prefer a less invasive, conservative therapeutic approach. Furthermore, the relatively low emphasis (paroxysmal AF, 33%; persistent AF, 29%) on lifestyle improvements and risk factor management suggests that these aspects warrant more attention. In terms of antiarrhythmic drugs, 73% of physicians utilized class Ic drugs, while 22% chose amiodarone. The use of colchicine was reported by 13% of the physicians.
CONCLUSIONS
- Although AF recurrence is a prevalent and complex problem, there are few guidelines for its management. This paper reviews past literature, recent studies, and trends concerning the mechanisms and management of AF recurrences. While PV reconnection is indeed a significant mechanism that triggers and sustains AF recurrence, it does not account for all instances of recurrence. Consequently, personalized management strategies, tailored to individual characteristics, are crucial for successful long-term outcomes in AF patients following catheter ablation. Further research is required to optimize therapeutic approaches for AF recurrence.
ARTICLE INFORMATION
-
Ethics statements
Not applicable.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: HKJ; Supervision: NHK, JSK, SSK; Writing–original draft: HKJ; Writing–review & editing: all authors. All authors read and approved the final manuscript.
Fig. 1.Mechanism of recurrence of atrial tachyarrhythmias according to the recurrence period. PV, pulmonary vein; SVC, superior vena cava; RA, right atrium; MA, mitral annulus; CT, crista terminalis; LA, left atrium; PW, posterior wall; AW, anterior wall; LAA, left atrium appendage; CS, coronary sinus; VOM, vein of Marshal.
REFERENCES
- 1. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 2021;42:373–498.ArticlePubMed
- 2. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–962.ArticlePubMed
- 3. Kirchhof P, Camm AJ, Goette A, Brandes A, Eckardt L, Elvan A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 2020;383:1305–16.ArticlePubMed
- 4. Haissaguerre M, Jais P, Shah DC, Takahashi A, Hocini M, Quiniou G, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 1998;339:659–66.ArticlePubMed
- 5. Andrade JG, Wells GA, Deyell MW, Bennett M, Essebag V, Champagne J, et al. Cryoablation or drug therapy for initial treatment of atrial fibrillation. N Engl J Med 2021;384:305–15.ArticlePubMed
- 6. Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med 2012;367:1587–95.ArticlePubMed
- 7. Poole JE, Bahnson TD, Monahan KH, Johnson G, Rostami H, Silverstein AP, et al. Recurrence of atrial fibrillation after catheter ablation or antiarrhythmic drug therapy in the CABANA Trial. J Am Coll Cardiol 2020;75:3105–18.ArticlePubMedPMC
- 8. Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 2018;20:e1–160.Article
- 9. Choi JI, Pak HN, Park JS, Kwak JJ, Nagamoto Y, Lim HE, et al. Clinical significance of early recurrences of atrial tachycardia after atrial fibrillation ablation. J Cardiovasc Electrophysiol 2010;21:1331–7.ArticlePubMed
- 10. Arya A, Hindricks G, Sommer P, Huo Y, Bollmann A, Gaspar T, et al. Long-term results and the predictors of outcome of catheter ablation of atrial fibrillation using steerable sheath catheter navigation after single procedure in 674 patients. Europace 2010;12:173–80.ArticlePubMed
- 11. Verma A, Mantovan R, Macle L, De Martino G, Chen J, Morillo CA, et al. Substrate and Trigger Ablation for Reduction of Atrial Fibrillation (STAR AF): a randomized, multicentre, international trial. Eur Heart J 2010;31:1344–56.ArticlePubMedPMC
- 12. Oral H, Knight BP, Ozaydin M, Tada H, Chugh A, Hassan S, et al. Clinical significance of early recurrences of atrial fibrillation after pulmonary vein isolation. J Am Coll Cardiol 2002;40:100–4.ArticlePubMed
- 13. Lee SH, Tai CT, Hsieh MH, Tsai CF, Lin YK, Tsao HM, et al. Predictors of early and late recurrence of atrial fibrillation after catheter ablation of paroxysmal atrial fibrillation. J Interv Card Electrophysiol 2004;10:221–6.ArticlePubMed
- 14. Grubman E, Pavri BB, Lyle S, Reynolds C, Denofrio D, Kocovic DZ. Histopathologic effects of radiofrequency catheter ablation in previously infarcted human myocardium. J Cardiovasc Electrophysiol 1999;10:336–42.ArticlePubMed
- 15. Hsieh MH, Chiou CW, Wen ZC, Wu CH, Tai CT, Tsai CF, et al. Alterations of heart rate variability after radiofrequency catheter ablation of focal atrial fibrillation originating from pulmonary veins. Circulation 1999;100:2237–43.ArticlePubMed
- 16. Fenelon G, Brugada P. Delayed effects of radiofrequency energy: mechanisms and clinical implications. Pacing Clin Electrophysiol 1996;19(4 Pt 1):484–9.Article
- 17. Kim YG, Boo KY, Choi JI, Choi YY, Choi HY, Roh SY, et al. Early recurrence is reliable predictor of late recurrence after radiofrequency catheter ablation of atrial fibrillation. JACC Clin Electrophysiol 2021;7:343–51.ArticlePubMed
- 18. Willems S, Khairy P, Andrade JG, Hoffmann BA, Levesque S, Verma A, et al. Redefining the blanking period after catheter ablation for paroxysmal atrial fibrillation: insights from the ADVICE (Adenosine Following Pulmonary Vein Isolation to Target Dormant Conduction Elimination) trial. Circ Arrhythm Electrophysiol 2016;9:e003909.ArticlePubMed
- 19. Andrade JG, Macle L, Khairy P, Khaykin Y, Mantovan R, De Martino G, et al. Incidence and significance of early recurrences associated with different ablation strategies for AF: a STAR-AF substudy. J Cardiovasc Electrophysiol 2012;23:1295–301.ArticlePubMed
- 20. Park CS, Kim H, Lee SR, Lee JH, Cho Y, Choi EK, et al. Prognostic implication of early recurrence after cryoballoon ablation in patients with atrial fibrillation. J Interv Card Electrophysiol 2023 May 1 [Epub]. https://doi.org/10.1007/s10840-023-01555-3.ArticlePubMed
- 21. Themistoclakis S, Schweikert RA, Saliba WI, Bonso A, Rossillo A, Bader G, et al. Clinical predictors and relationship between early and late atrial tachyarrhythmias after pulmonary vein antrum isolation. Heart Rhythm 2008;5:679–85.ArticlePubMed
- 22. Onishi N, Kaitani K, Nakagawa Y, Inoue K, Kobori A, Nakazawa Y, et al. The association between late-phase early recurrence within the blanking period after atrial fibrillation catheter ablation and long-term recurrence: insights from a large-scale multicenter study. Int J Cardiol 2021;341:39–45.ArticlePubMed
- 23. Popa MA, Kottmaier M, Risse E, Telishevska M, Lengauer S, Wimbauer K, et al. Early arrhythmia recurrence after catheter ablation for persistent atrial fibrillation: is it predictive for late recurrence? Clin Res Cardiol 2022;111:85–95.ArticlePubMedPMCPDF
- 24. Weerasooriya R, Khairy P, Litalien J, Macle L, Hocini M, Sacher F, et al. Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow-up? J Am Coll Cardiol 2011;57:160–6.ArticlePubMed
- 25. Tzou WS, Marchlinski FE, Zado ES, Lin D, Dixit S, Callans DJ, et al. Long-term outcome after successful catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol 2010;3:237–42.ArticlePubMed
- 26. Jais P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation 2008;118:2498–505.ArticlePubMed
- 27. Calkins H, Reynolds MR, Spector P, Sondhi M, Xu Y, Martin A, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol 2009;2:349–61.ArticlePubMed
- 28. Vidal-Perez R, Otero-Ravina F, Lado-Lopez M, Turrado-Turrado V, Rodriguez-Moldes E, Gomez-Vazquez JL, et al. The change in the atrial fibrillation type as a prognosis marker in a community study: long-term data from AFBAR (Atrial Fibrillation in the BARbanza) study. Int J Cardiol 2013;168:2146–52.ArticlePubMed
- 29. de Vos CB, Pisters R, Nieuwlaat R, Prins MH, Tieleman RG, Coelen RJ, et al. Progression from paroxysmal to persistent atrial fibrillation clinical correlates and prognosis. J Am Coll Cardiol 2010;55:725–31.ArticlePubMed
- 30. Hobbelt AH, Spronk HM, Crijns HJ, Ten Cate H, Rienstra M, Van Gelder IC. Prethrombotic state in young very low-risk patients with atrial fibrillation. J Am Coll Cardiol 2017;69:1990–2.ArticlePubMed
- 31. Habibi M, Samiei S, Ambale Venkatesh B, Opdahl A, Helle-Valle TM, Zareian M, et al. Cardiac magnetic resonance-measured left atrial volume and function and incident atrial fibrillation: results from MESA (Multi-Ethnic Study of Atherosclerosis). Circ Cardiovasc Imaging 2016;9:10.1161/CIRCIMAGING.115.004299 e004299. ArticlePubMedPMC
- 32. Brambatti M, Connolly SJ, Gold MR, Morillo CA, Capucci A, Muto C, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation 2014;129:2094–9.ArticlePubMed
- 33. Guichard JB, Nattel S. Atrial cardiomyopathy: a useful notion in cardiac disease management or a passing fad? J Am Coll Cardiol 2017;70:756–65.ArticlePubMed
- 34. Wokhlu A, Hodge DO, Monahan KH, Asirvatham SJ, Friedman PA, Munger TM, et al. Long-term outcome of atrial fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol 2010;21:1071–8.ArticlePubMed
- 35. Sotomi Y, Inoue K, Ito N, Kimura R, Toyoshima Y, Masuda M, et al. Cause of very late recurrence of atrial fibrillation or flutter after catheter ablation for atrial fibrillation. Am J Cardiol 2013;111:552–6.ArticlePubMed
- 36. Shah S, Barakat AF, Saliba WI, Abdur Rehman K, Tarakji KG, Rickard J, et al. Recurrent atrial fibrillation after initial long-term ablation success: electrophysiological findings and outcomes of repeat ablation procedures. Circ Arrhythm Electrophysiol 2018;11:e005785.ArticlePubMed
- 37. Erhard N, Mauer T, Ouyang F, Sciacca V, Rillig A, Reissmann B, et al. Mechanisms of late arrhythmia recurrence after initially successful pulmonary vein isolation in patients with atrial fibrillation. Pacing Clin Electrophysiol 2023;46:161–8.ArticlePubMedPDF
- 38. Choi SH, Yu HT, Kim D, Park JW, Kim TH, Uhm JS, et al. Late recurrence of atrial fibrillation 5 years after catheter ablation: predictors and outcome. Europace 2023;25:euad113.ArticlePubMedPMCPDF
- 39. Gaztanaga L, Frankel DS, Kohari M, Kondapalli L, Zado ES, Marchlinski FE. Time to recurrence of atrial fibrillation influences outcome following catheter ablation. Heart Rhythm 2013;10:2–9.ArticlePubMed
- 40. Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, et al. Relationship between pulmonary vein reconnection and atrial fibrillation recurrence: a systematic review and meta-analysis. JACC Clin Electrophysiol 2016;2:474–83.ArticlePubMed
- 41. D’Ascenzo F, Corleto A, Biondi-Zoccai G, Anselmino M, Ferraris F, di Biase L, et al. Which are the most reliable predictors of recurrence of atrial fibrillation after transcatheter ablation?: a meta-analysis. Int J Cardiol 2013;167:1984–9.ArticlePubMed
- 42. Berruezo A, Tamborero D, Mont L, Benito B, Tolosana JM, Sitges M, et al. Pre-procedural predictors of atrial fibrillation recurrence after circumferential pulmonary vein ablation. Eur Heart J 2007;28:836–41.ArticlePubMed
- 43. Nedios S, Kosiuk J, Koutalas E, Kornej J, Sommer P, Arya A, et al. Comparison of left atrial dimensions in CT and echocardiography as predictors of long-term success after catheter ablation of atrial fibrillation. J Interv Card Electrophysiol 2015;43:237–44.ArticlePubMedPDF
- 44. Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D, et al. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace 2018;20:33–42.ArticlePubMed
- 45. Costa FM, Ferreira AM, Oliveira S, Santos PG, Durazzo A, Carmo P, et al. Left atrial volume is more important than the type of atrial fibrillation in predicting the long-term success of catheter ablation. Int J Cardiol 2015;184:56–61.ArticlePubMed
- 46. Chao TF, Hung CL, Tsao HM, Lin YJ, Yun CH, Lai YH, et al. Epicardial adipose tissue thickness and ablation outcome of atrial fibrillation. PLoS One 2013;8:e74926.ArticlePubMedPMC
- 47. Hirota K, Fukui A, Yamaguchi T, Takahashi M, Kondo H, Akioka H, et al. Interatrial conduction time is associated with left atrial low voltage area and predicts the recurrence after single atrial fibrillation ablation. J Arrhythm 2023;39:142–8.ArticlePubMedPMCPDF
- 48. Vinter N, Calvert P, Kronborg MB, Cosedis-Nielsen J, Gupta D, Ding WY, et al. Social determinants of health and recurrence of atrial fibrillation after catheter ablation: a Danish nationwide cohort study. Eur Heart J Qual Care Clin Outcomes 2023;9:632–8.ArticlePubMedPDF
- 49. Intzes S, Zagoridis K, Symeonidou M, Spanoudakis E, Arya A, Dinov B, et al. P-wave duration and atrial fibrillation recurrence after catheter ablation: a systematic review and meta-analysis. Europace 2023;25:450–9.ArticlePubMedPMCPDF
- 50. Chae S, Oral H, Good E, Dey S, Wimmer A, Crawford T, et al. Atrial tachycardia after circumferential pulmonary vein ablation of atrial fibrillation: mechanistic insights, results of catheter ablation, and risk factors for recurrence. J Am Coll Cardiol 2007;50:1781–7.ArticlePubMed
- 51. Castrejon-Castrejon S, Ortega M, Perez-Silva A, Doiny D, Estrada A, Filgueiras D, et al. Organized atrial tachycardias after atrial fibrillation ablation. Cardiol Res Pract 2011;2011:957538. ArticlePubMedPMC
- 52. Choi Y, Kim S, Baek JY, Kim SH, Kim JY, Kim TS, et al. Acute and long-term outcome of redo catheter ablation for recurrent atrial tachycardia and recurrent atrial fibrillation in patients with prior atrial fibrillation ablation. J Interv Card Electrophysiol 2021;61:227–34.ArticlePubMedPDF
- 53. Gerstenfeld EP, Callans DJ, Dixit S, Russo AM, Nayak H, Lin D, et al. Mechanisms of organized left atrial tachycardias occurring after pulmonary vein isolation. Circulation 2004;110:1351–7.ArticlePubMed
- 54. Leong-Sit P, Roux JF, Zado E, Callans DJ, Garcia F, Lin D, et al. Antiarrhythmics after ablation of atrial fibrillation (5A Study): six-month follow-up study. Circ Arrhythm Electrophysiol 2011;4:11–4.ArticlePubMed
- 55. Darkner S, Chen X, Hansen J, Pehrson S, Johannessen A, Nielsen JB, et al. Recurrence of arrhythmia following short-term oral AMIOdarone after CATheter ablation for atrial fibrillation: a double-blind, randomized, placebo-controlled study (AMIO-CAT trial). Eur Heart J 2014;35:3356–64.ArticlePubMed
- 56. Kaitani K, Inoue K, Kobori A, Nakazawa Y, Ozawa T, Kurotobi T, et al. Efficacy of Antiarrhythmic Drugs Short-Term Use After Catheter Ablation for Atrial Fibrillation (EAST-AF) trial. Eur Heart J 2016;37:610–8.ArticlePubMed
- 57. Goldenberg GR, Burd D, Lodzinski P, Stabile G, Udell JA, Newman D, et al. Antiarrhythmic therapy as an adjuvant to promote post pulmonary vein isolation success: a meta-analysis. J Interv Card Electrophysiol 2016;47:171–6.ArticlePubMedPDF
- 58. Kim YR, Nam GB, Han S, Kim SH, Kim KH, Lee S, et al. Effect of short-term steroid therapy on early recurrence during the blanking period after catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol 2015;8:1366–72.ArticlePubMed
- 59. Iskandar S, Reddy M, Afzal MR, Rajasingh J, Atoui M, Lavu M, et al. Use of oral steroid and its effects on atrial fibrillation recurrence and inflammatory cytokines post ablation: the steroid AF study. J Atr Fibrillation 2017;9:1604. ArticlePubMedPMC
- 60. Deftereos S, Giannopoulos G, Kossyvakis C, Efremidis M, Panagopoulou V, Kaoukis A, et al. Colchicine for prevention of early atrial fibrillation recurrence after pulmonary vein isolation: a randomized controlled study. J Am Coll Cardiol 2012;60:1790–6.ArticlePubMed
- 61. Deftereos S, Giannopoulos G, Efremidis M, Kossyvakis C, Katsivas A, Panagopoulou V, et al. Colchicine for prevention of atrial fibrillation recurrence after pulmonary vein isolation: mid-term efficacy and effect on quality of life. Heart Rhythm 2014;11:620–8.ArticlePubMed
- 62. Yue H, Liang W, Zhan Y, Zhang Z, Qin X, Bian L, et al. Colchicine: emerging therapeutic effects on atrial fibrillation by alleviating myocardial fibrosis in a rat model. Biomed Pharmacother 2022;154:113573. ArticlePubMed
- 63. Agarwal S, Munir MB, Asad ZUA. Safety and efficacy of colchicine for the prevention of recurrent atrial fibrillation post-catheter ablation: colchicine for recurrent AF post-PVI. Eur J Intern Med 2023;111:143–5.ArticlePubMed
- 64. O’Donnell D, Furniss SS, Dunuwille A, Bourke JP. Delayed cure despite early recurrence after pulmonary vein isolation for atrial fibrillation. Am J Cardiol 2003;91:83–5.ArticlePubMed
- 65. Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation: a study in awake chronically instrumented goats. Circulation 1995;92:1954–68.ArticlePubMed
- 66. von Olshausen G, Paul-Nordin A, Tapanainen J, Jensen-Urstad M, Bastani H, Saluveer O, et al. Electrical cardioversion for early recurrences post pulmonary vein isolation. J Interv Card Electrophysiol 2023;66:577–84.ArticlePubMedPMC
- 67. Malasana G, Day JD, Weiss JP, Crandall BG, Bair TL, May HT, et al. A strategy of rapid cardioversion minimizes the significance of early recurrent atrial tachyarrhythmias after ablation for atrial fibrillation. J Cardiovasc Electrophysiol 2011;22:761–6.ArticlePubMed
- 68. Ebert M, Stegmann C, Kosiuk J, Dinov B, Richter S, Arya A, et al. Predictors, management, and outcome of cardioversion failure early after atrial fibrillation ablation. Europace 2018;20:1428–34.ArticlePubMed
- 69. Chilukuri K, Dukes J, Dalal D, Marine JE, Henrikson CA, Scherr D, et al. Outcomes in patients requiring cardioversion following catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol 2010;21:27–32.ArticlePubMed
- 70. Mujovic N, Marinkovic M, Markovic N, Vucicevic V, Lip GY, Bunch TJ, et al. The relationship of early recurrence of atrial fibrillation and the 3-month integrity of the ablation lesion set. Sci Rep 2018;8:9875. ArticlePubMedPMC
- 71. Lellouche N, Jais P, Nault I, Wright M, Bevilacqua M, Knecht S, et al. Early recurrences after atrial fibrillation ablation: prognostic value and effect of early reablation. J Cardiovasc Electrophysiol 2008;19:599–605.ArticlePubMed
- 72. Andrade JG, Khairy P, Macle L, Packer DL, Lehmann JW, Holcomb RG, et al. Incidence and significance of early recurrences of atrial fibrillation after cryoballoon ablation: insights from the multicenter Sustained Treatment of Paroxysmal Atrial Fibrillation (STOP AF) trial. Circ Arrhythm Electrophysiol 2014;7:69–75.ArticlePubMed
- 73. Wasmer K, Dechering DG, Kobe J, Monnig G, Pott C, Frommeyer G, et al. Pulmonary vein reconnection and arrhythmia progression after antral linear catheter ablation of paroxysmal and persistent atrial fibrillation. Clin Res Cardiol 2016;105:738–43.ArticlePubMedPDF
- 74. Park JW, Yu HT, Kim TH, Uhm JS, Joung B, Lee MH, et al. Mechanisms of long-term recurrence 3 years after catheter ablation of atrial fibrillation. JACC Clin Electrophysiol 2020;6:999–1007.ArticlePubMed
- 75. Kim YG, Choi HY, Shim J, Min K, Choi YY, Choi JI, et al. Electrical remodeling of left atrium is a better predictor for recurrence than structural remodeling in atrial fibrillation patients undergoing radiofrequency catheter ablation. Korean Circ J 2022;52:368–78.ArticlePubMedPDF
- 76. Zhou L, He L, Wang W, Li C, Li S, Tang R, et al. Effect of repeat catheter ablation vs. antiarrhythmic drug therapy among patients with recurrent atrial tachycardia/atrial fibrillation after atrial fibrillation catheter ablation: data from CHINA-AF registry. Europace 2023;25:382–9.ArticlePubMedPMCPDF
- 77. Friberg L, Tabrizi F, Englund A. Catheter ablation for atrial fibrillation is associated with lower incidence of stroke and death: data from Swedish health registries. Eur Heart J 2016;37:2478–87.ArticlePubMed
- 78. Holmqvist F, Simon D, Steinberg BA, Hong SJ, Kowey PR, Reiffel JA, et al. Catheter ablation of atrial fibrillation in U.S. community practice: results from Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). J Am Heart Assoc 2015;4:e001901.ArticlePubMedPMC
- 79. Al-Hijji MA, Deshmukh AJ, Yao X, Mwangi R, Sangaralingham LR, Friedman PA, et al. Trends and predictors of repeat catheter ablation for atrial fibrillation. Am Heart J 2016;171:48–55.ArticlePubMed
- 80. Bordignon S, Barra S, Providencia R, de Asmundis C, Marijon E, Farkowski MM, et al. The blanking period after atrial fibrillation ablation: an European Heart Rhythm Association survey on contemporary definition and management. Europace 2022;24:1684–90.ArticlePubMedPDF
- 81. Schwab AC, Anic A, Farkowski MM, Guerra J, Iliodromitis KE, Jubele K, et al. Rhythm monitoring, success definition, recurrence, and anticoagulation after atrial fibrillation ablation: results from an EHRA survey. Europace 2023;25:676–81.ArticlePubMedPMCPDF
Citations
Citations to this article as recorded by

 , Sung Soo Kim2
, Sung Soo Kim2 , Hyung Ki Jeong1
, Hyung Ki Jeong1 , Nam Ho Kim1
, Nam Ho Kim1