ABSTRACT
- Remote collaborative care is a program that improves medical services by linking local and remote physicians with residents in areas where access to medical facilities is limited, utilizing information and communication technology. As a result, patients can obtain medical advice and counseling at local hospitals without needing to travel to distant facilities. This care model involves communication between doctors, facilitating the accurate transfer of medical information and reducing the risk of misunderstandings. For instance, managing conditions such as blood pressure or blood glucose is more straightforward because a local hospital can assess the patient's status while a remote hospital simultaneously provides high-quality, specialized medical services. With the rise in poorly controlled hypertension or diabetes, the need for remote collaborative care has also increased. This care model enables local hospitals to maintain continuous patient care with the support of remote facilities. This is particularly true following acute cardiovascular treatment, where local hospitals, assisted by remote institutions, can safely offer high-quality services such as rehabilitation and follow-up care. Although remote hospitals have many advantages with the increasing number of patients, many difficulties remain in commercializing unsystematized remote collaborative care. Specifically, low reimbursements for medical services must be addressed, proper equipment is needed, more time and effort must be invested, and the liability issue must also be dealt with. Nevertheless, remote collaborative care using information and communication technology will be necessary in the future. Medical staff need to objectively examine the advantages and disadvantages of remote collaborative care from various perspectives and find ways to revitalize it.
-
Keywords: Communication; Hypertension; Information technology; Telemedicine
INTRODUCTION
- Telehealth, also known as telemedicine and telemonitoring, continues to be an important issue in the medical field [1–3]. In particular, blood pressure and blood glucose levels, which may fluctuate depending on the situation, can be managed remotely without requiring the patient to visit a large university hospital [4,5]. Telehealth is also helpful for postoperative wound management or rehabilitation after cardiocerebrovascular disease [6,7]. Unlike telemedicine, which involves a patient-doctor relationship [8], remote collaborative care involves a doctor-doctor relationship and is expected to help patients immensely as virtual communication is smoother. Despite its advantages, remote collaborative care has garnered relatively little attention and remains unfamiliar to many.
- In remote collaborative care, a doctor located at a distance provides guidance on medical procedures to a local physician [9]. This approach aims to minimize unnecessary patient transfers while preserving the standard of medical services between urban centers and medically underserved regions through collaborative efforts among doctors [10]. The primary goal is to maintain a level of quality similar to that of in-hospital collaborative care at university hospitals and to ensure that people in medically underserved areas receive high-quality medical services [11]. Ultimately, it is considered a realistic solution that can solve the lack of resources in medically underserved areas and urban concentration of medical institutions. In addition, this approach is expected to improve the quality and competitiveness of small local medical institutions. Despite the well-meaning goals of remote collaborative care, it is necessary to determine why physicians are hesitant to use it in clinical practice.
FROM THE PATIENT’S PERSPECTIVE
- Advantages
Improved patient convenience without restrictions on time and space
- Patients can receive local treatment from remote specialists without the need to travel to a large city (Fig. 1). This approach can reduce both the time and expenses for patients, while also improving their access to treatment [11]. The ability to receive expert medical care irrespective of geographical location and time offers significant benefits, particularly for postoperative health management and the care of cancer patients [6,7]. Additionally, patients who have been treated for various acute cardiovascular conditions, such as myocardial infarction, cerebral infarction, or stroke, can continue their recovery at home without the burden of unnecessary travel [12,13]. Consequently, patients have the opportunity to undergo examinations and receive specialist consultations at remote hospitals during visits to their local healthcare facilities.
Availability of high-quality medical services in medically underserved areas
- Remote collaborative care is of paramount importance in the domestic medical market, which faces a shortage of personnel in certain treatment areas and a growing disparity in medical services between regions [10]. This approach enables the delivery of high-quality medical services in regional areas, including small towns and islands [11]. By increasing the utilization of medical resources, remote collaborative care is anticipated to mitigate issues related to resource scarcity and the concentration of services in local medical institutions. In particular, for chronic conditions such as uncontrolled hypertension or diabetes, consistent treatment at a nursing hospital, primary clinic, or public health center in a medically underserved area is advisable [14].
- Disadvantages
- The accessibility of medical care is extremely high in Korea [15]. Therefore, patients who are dissatisfied with their local medical institutions frequently seek care directly from remote medical institutions. This behavior can inadvertently undermine the original intent of remote collaborative care. Moreover, there is a concern that patients' trust in their local doctors may diminish if their local hospital is perceived as reliant on collaborative care from a remote hospital, potentially causing patient anxiety. At the same time, this dynamic may create trust issues among local doctors regarding their participation in remote collaborative care. Given that conditions such as hypertension and diabetes are commonly managed at primary clinics, it is necessary to broaden the scope to include consultations for complications related to cardiovascular disease.
FROM THE LOCAL MEDICAL INSTITUTION’S PERSPECTIVE
- Advantages
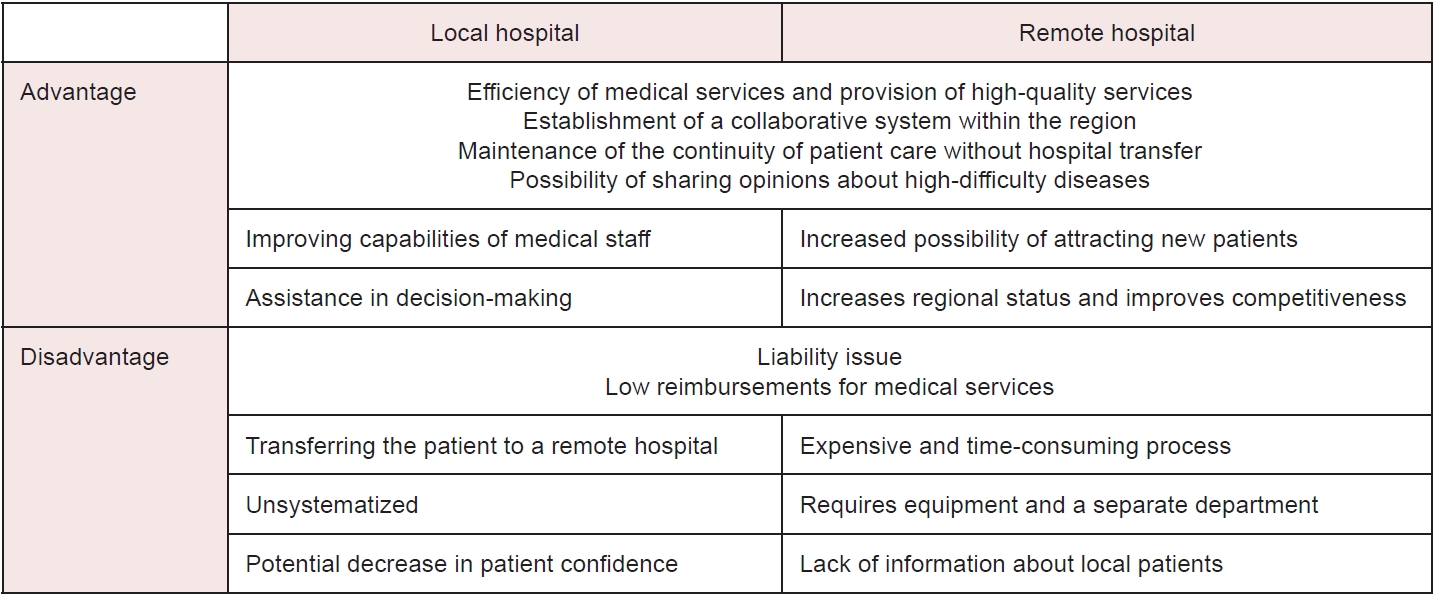
- The scope of patient care can be expanded through remote collaborative care, enabling local physicians to enhance their medical capabilities [16]. This approach facilitates the implementation of patient-centered care and elevates the standard of local medical facilities. When faced with diseases outside their area of expertise, local doctors can seek expert treatment advice from colleagues at distant hospitals, thus reinforcing their role in patient care (Fig. 2). Consequently, local hospitals without specialized services can still offer high-quality medical care by consulting with remote institutions. Moreover, such collaboration allows for routine management following the acute treatment of cardiovascular diseases, promoting the continuity of care [12,13].
- In local medical institutions that do not have skilled medical staff or specialists for specific diseases, local physicians can receive help during emergencies. However, effective collaboration between remote medical staff and medical institutions is necessary to facilitate remote collaborative care in such critical situations [5]. Ultimately, the success of remote collaborative care depends on collaboration between remote medical institutions, which can also confer a competitive edge to local medical facilities.
- Disadvantages
Lack of proactiveness from local medical institutions
- Requesting remote collaborative care from a doctor who is not local reflects the local doctor's lack of medical specialization. Local doctors may feel pressured to seek a second opinion because they are concerned about patients' perceived lack of trust in their capabilities, which can arise during the process of remote collaborative care. There is a common misconception during remote collaborative care that if medical treatment is administered in real-time under the guidance of a remote doctor, the local doctor is seeking external assistance due to a deficiency in his or her professional skills. Consequently, patients may struggle to regard them as competent medical professionals. This misunderstanding can undermine the patient-doctor relationship, which is built on trust, and ultimately diminish local doctors' self-esteem. As a result, local medical institutions may be hesitant to engage actively in remote collaborative care.
The question of liability
- In remote collaborative care, the local doctor must trust the decisions of the remote doctor. If the results differ from expectations (or if the local and remote doctors have different opinions), liability issues arise [17]. Furthermore, if the local doctor administers the appropriate treatment based on the remote doctor's directives, liability issues may still surface in the event of adverse outcomes.
Miscellaneous
- Patients may leave local hospitals and visit remote tertiary hospitals. This is impractical unless medical fees are raised to realistically reflect the associated costs. It is difficult to implement a platform for conveying patients’ personal information, photographs, test results, and so on.
FROM THE REMOTE MEDICAL INSTITUTION’S PERSPECTIVE
- Advantages
- Building close relationships with local medical institutions facilitates the referral of patients with severe diseases. This approach offers a distinct advantage by potentially securing a new patient demographic. Specifically, it is often challenging for patients to commute to a distant hospital for follow-up care after initial treatment of acute conditions such as cancer, myocardial infarction, and stroke [12,13,18]. In such instances, the distant hospital can obtain updates on the patient's condition from the local hospital, enabling it to provide accurate consultations and advice.
- Therefore, the role of medical institutions in delivering healthcare services is likely to expand. Remote collaborative care increases the trustworthiness of distant hospitals by offering specialized medical services to patients at local facilities. By improving the quality of local healthcare, we can strengthen the reputation of these community hospitals.
- Remote collaborative care involves an exchange of opinions between doctors; therefore, the possibility of misunderstandings in communication is less likely to occur. After treatment for acute cardiocerebrovascular disease, effective communication among medical staff is essential. Consequently, this communication process differs markedly from that of non–face-to-face treatments [19].
- Disadvantages
Profit problems
- In Korea, the returns on remote collaborative care are low relative to the time, effort, and cost invested [20]. This is attributed to the fact that specialists in remote hospitals are not assured of adequate profits. Given that non–face-to-face patients require more information to be gathered for a comprehensive understanding of their issues, and that secondary advice is also provided, the profits generated are insufficient.
Liability issues
- Understanding the detailed condition of local patients and their specific medical situation can be challenging from a remote hospital. There is an inherent risk in making medical decisions based solely on a local doctor's assessment of the patient's condition without an in-person consultation. Consequently, this can lead to distrust and result in patients being referred to a remote hospital following acute treatment for cardiovascular disease.
Need for a remote platform
- Several medical resources (budget, human resources, systems, etc.) must be accessed for remote collaborative care [8]. Given the need to share, transmit, and receive patient information among medical staff in remote settings, the creation and utilization of a medical information system are imperative [21]. Furthermore, it is crucial to establish standards for system development that promote communication among medical professionals. This includes standardization between hospitals, interoperability, and the protection of information [22]. Even if such a system is implemented, the medical quality of local hospitals needs to be improved; regrettably, this often does not happen in practice.
Miscellaneous
- If a disease requires remote collaborative care, many patients go directly to a local hospital to request such care and proper treatment. Remote hospitals may have insufficient time and workload to handle remote collaborative care. Thus, there is a need to designate a new person in charge of communication with the local hospital and other work roles.
SUGGESTIONS FOR PROMOTING REMOTE COLLABORATIVE CARE
- The usefulness and effectiveness of various telemedicine and telemonitoring methods to manage chronic diseases—such as hypertension, diabetes, and obesity—have been proven on scientific grounds [23]. However, in managing these chronic diseases, remote collaborative care, which involves a doctor-doctor relationship, seems to be more helpful than telemedicine, which involves a patient-doctor relationship. Remote collaborative care is the only legal patient management system for telehealth in Korea [24]. It is helpful for managing the health of patients in medically underserved areas [10,11]. However, it is relatively unfamiliar and is not commercially available.
- To promote remote collaborative care, the top priority is selecting suitable target patients, diseases, and regions. University hospitals have already begun to explore multidisciplinary approaches for complex diseases and challenging diagnostic and treatment cases [5]. For remote collaborative care to gain a competitive edge, it should prioritize special cases. Moreover, it would be advantageous to highlight its application in medical fields experiencing a shortage of specialists, such as pediatrics, burn care, and rehabilitation. Chronic conditions like hypertension and obesity, which have shown positive outcomes with telemedicine, stand to benefit significantly from remote collaborative care. Many patients with poorly controlled hypertension and diabetes [5] require more intensive management from specialists. Since managing acute diseases after procedures is critical in remote hospitals [12,13], promoting doctor-to-doctor relationships in remote collaborative care could yield substantial social benefits.
- The work processes of both local and remote hospitals must be standardized, necessitating the development of operating guidelines [8]. Information is needed regarding which hospitals are in remote locations and which diseases are eligible for remote collaborative care. Remote hospitals must provide reasonable operating policies regarding the dates, times, departments, and attending physicians for remote collaborative care. Therefore, a plan is required to achieve remote collaborative care without substantially disrupting the existing processes of remote hospitals. Furthermore, it would be helpful to categorize instances in which remote collaborative care is required at local hospitals.
- Therefore, a system (or platform) that connects local and remote hospitals is required, one that facilitates free and efficient remote collaborative care. Continuous cooperation between local and remote hospitals is essential, necessitating the establishment of a system that allows immediate contact with specialists for specific diseases to ensure uninterrupted regular operations. Patient information, including test results from local hospitals, must be clearly displayed at remote hospitals. Furthermore, the complexity and technical challenges associated with remote collaborative care systems must be addressed. There are already many medical platforms targeting people at high risk of cardiovascular diseases, such as those with hypertension [25]. It is important to explore how these platforms can be utilized for medical treatment. Platform performance is known to significantly impact patient health [26].
- Although remote collaborative care is a legitimate healthcare system, it remains relatively unfamiliar to both patients and doctors [24]. Therefore, there is a need to highlight the need for remote collaborative care, rather than mandating its adoption. The government could emphasize the need for remote collaborative care for patients, and it would be beneficial to highlight the advantages for local and remote hospitals discussed above. The ultimate goal would be to improve the awareness of patients, local doctors, and remote doctors by promoting the necessity and usefulness of remote collaborative care.
- Finally, the government should support fee increases or incentives for local and remote doctors to preserve their profit structures. This support is necessary because hospitals require time and medical compensation for remote collaborative care (i.e., there must be more benefits than referring patients to remote locations).
- Despite these challenges, remote collaborative care presents a viable alternative that necessitates active participation from local medical institutions, particularly in an aging society grappling with chronic conditions such as diabetes. However, there exists a significant disparity between the ideal benefits and the practical advantages as perceived by patients, local hospitals, and remote hospitals. In an era where remote collaborative care is increasingly becoming a global norm, it is crucial to understand the specific demands and needs of patients, local physicians, and remote physicians. If Korea, which is recognized as an information technology powerhouse, effectively harnesses the potential of remote collaborative care, it has the opportunity to solidify its position as an unrivaled leader in medical advancement within Asia. This moment calls for boundless engagement and dedication.
ARTICLE INFORMATION
-
Author contributions
Conceptualization: SYB, HSK; Formal analysis: all authors; Funding acquisition: HSK; Investigation: HSK; Methodology: HSK; Project administration: HSK; Resources: HSK; Software: SYB, HSK; Supervision: HSK; Validation: HSK; Visualization: SYB; Writing–original draft: SYB; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
This study was supported by a grant for the Teleconsultation in Medically Underserved Areas (MUAs), funded by the Korean Ministry of Health and Welfare.
Fig. 1.Realistic example of remote collaborative care.
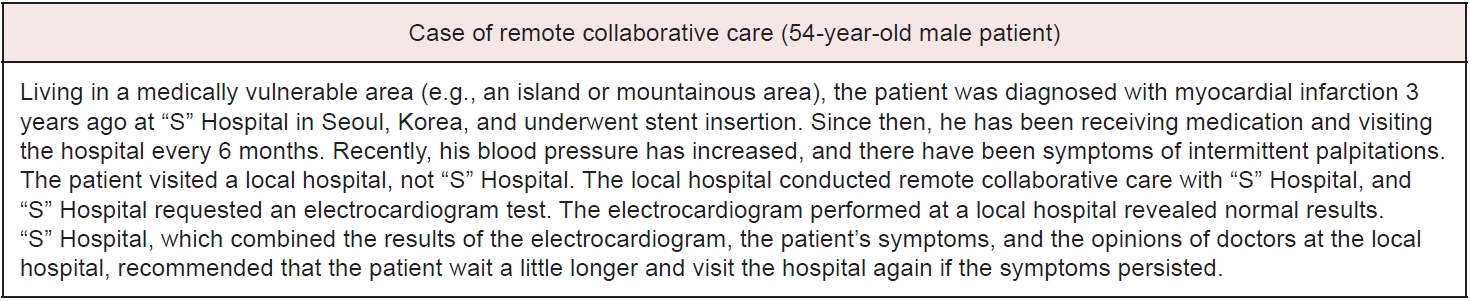
Fig. 2.Advantages and disadvantages of remote collaborative care.
REFERENCES
- 1. Snoswell CL, Chelberg G, De Guzman KR, Haydon HH, Thomas EE, Caffery LJ, et al. The clinical effectiveness of telehealth: a systematic review of meta-analyses from 2010 to 2019. J Telemed Telecare 2023;29:669–84.ArticlePubMedPDF
- 2. Snoswell CL, Stringer H, Taylor ML, Caffery LJ, Smith AC. An overview of the effect of telehealth on mortality: a systematic review of meta-analyses. J Telemed Telecare 2023;29:659–68.ArticlePubMedPDF
- 3. Pierce RP, Stevermer JJ. Disparities in the use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare 2023;29:3–9.ArticlePubMedPDF
- 4. Kim HS, Hwang Y, Lee JH, Oh HY, Kim YJ, Kwon HY, et al. Future prospects of health management systems using cellular phones. Telemed J E Health 2014;20:544–51.ArticlePubMedPMC
- 5. Kim HS, Sun C, Yang SJ, Sun L, Li F, Choi IY, et al. Randomized, open-label, parallel group study to evaluate the effect of internet-based glucose management system on subjects with diabetes in China. Telemed J E Health 2016;22:666–74.ArticlePubMed
- 6. Xiao K, Yeung JC, Bolger JC. The safety and acceptability of using telehealth for follow-up of patients following cancer surgery: a systematic review. Eur J Surg Oncol 2023;49:9–15.ArticlePubMedPMC
- 7. Kis A, Razek T, Grushka J, Boulanger N, Watt L, Deckelbaum D, et al. Surgical, trauma and telehealth capacity in Indigenous communities in Northern Quebec: a cross-sectional survey. Can J Surg 2023;66:E572–9.ArticlePubMedPMC
- 8. Kim HS. Towards telemedicine adoption in Korea: 10 practical recommendations for physicians. J Korean Med Sci 2021;36:e103.ArticlePubMedPMCPDF
- 9. Whitfield J, LePoire E, Stanczyk B, Ratzliff A, Cerimele JM. Remote collaborative care with off-site behavioral health care managers: a systematic review of clinical trials. J Acad Consult Liaison Psychiatry 2022;63:71–85.ArticlePubMed
- 10. Swar S, Rimal P, Gauchan B, Maru D, Yang Y, Acharya B. Delivering collaborative care in rural settings: integrating remote teleconsultation and local supervision in rural Nepal. Psychiatr Serv 2019;70:78–81.ArticlePubMedPMC
- 11. Rojas G, Guajardo V, Martinez P, Castro A, Fritsch R, Moessner M, et al. A remote collaborative care program for patients with depression living in rural areas: open-label trial. J Med Internet Res 2018;20:e158.ArticlePubMedPMC
- 12. Zerna C, Jeerakathil T, Hill MD. Telehealth for remote stroke management. Can J Cardiol 2018;34:889–96.ArticlePubMed
- 13. Wu Z, Xu J, Yue C, Li Y, Liang Y. Collaborative care model based telerehabilitation exercise training program for acute stroke patients in China: a randomized controlled trial. J Stroke Cerebrovasc Dis 2020;29:105328. ArticlePubMed
- 14. Curtis S, Martin H, DiNella M, Lavallee B, Chartrand C, McLeod L, et al. Kidney check point-of-care testing-furthering patient engagement and patient-centered care in Canada’s rural and remote indigenous communities: program report. Can J Kidney Health Dis 2021;8:20543581211003744. ArticlePubMedPMCPDF
- 15. Korean Ministry of Health and Welfare; Korea Institute for Health and Social Affairs. OECD health statistics 2022. Korean Ministry of Health and Welfare; 2023.
- 16. Hodgkins M, Barron M, Jevaji S, Lloyd S. Physician requirements for adoption of telehealth following the SARS-CoV-2 pandemic. NPJ Digit Med 2021;4:19. ArticlePubMedPMCPDF
- 17. Hyun DY. Legal regulations on telemedicine and their problems. Korean Soc Law Med 2022;23:3–33.Article
- 18. Jull J, Sheppard AJ, Hizaka A; Inuit Medical Interpreter Team, Barton G, Doering P, et al. Experiences of Inuit in Canada who travel from remote settings for cancer care and impacts on decision making. BMC Health Serv Res 2021;21:328. ArticlePubMedPMCPDF
- 19. Pan E, Cusack C, Hook J, Vincent A, Kaelber DC, Bates DW, et al. The value of provider-to-provider telehealth. Telemed J E Health 2008;14:446–53.ArticlePubMed
- 20. Song SY. [Why we don't do home-based medical care or visiting healthcare service? “It's lower than the outpatient profit”] [Internet]. The Korean Doctor's Weekly; 2023 [cited 2023 Nov 28]. Available from: https://www.docdocdoc.co.kr/news/articleView.html?idxno=3010822
- 21. Hayashi Y, Yokoyama Y, Kazama T, Hirayama D, Nakase H. Report on a new remote collaborative medical care system: construction and operation of a remote collaborative medical care network for inflammatory bowel disease using information and communication technology in Hokkaido. Nihon Shokakibyo Gakkai Zasshi 2022;119:830–8.ArticlePubMed
- 22. Tangari G, Ikram M, Ijaz K, Kaafar MA, Berkovsky S. Mobile health and privacy: cross sectional study. BMJ 2021;373:n1248. ArticlePubMedPMC
- 23. Kim HS, Yoon KH. Lessons from use of continuous glucose monitoring systems in digital healthcare. Endocrinol Metab (Seoul) 2020;35:541–8.ArticlePubMedPMCPDF
- 24. Korea Law Translation Center. Medical Service Act. Act No. 18468 (September 24, 2021), Article 34, Paragraph (1). Korea Legislation Research Institute; [updated 2023 Dec 20; cited 2023 Nov 28]. Available from: https://elaw.klri.re.kr/eng_service/lawView.do?hseq=64153&lang=ENG
- 25. Melillo P, Orrico A, Scala P, Crispino F, Pecchia L. Cloud-based smart health monitoring system for automatic cardiovascular and fall risk assessment in hypertensive patients. J Med Syst 2015;39:109. ArticlePubMedPDF
- 26. Kim HS, Choi W, Baek EK, Kim YA, Yang SJ, Choi IY, et al. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J 2014;38:204–10.ArticlePubMedPMC
Citations
Citations to this article as recorded by

 , Hakyoung Park2
, Hakyoung Park2 , Jiwon Shinn2
, Jiwon Shinn2 , Hun-Sung Kim2,3
, Hun-Sung Kim2,3
